
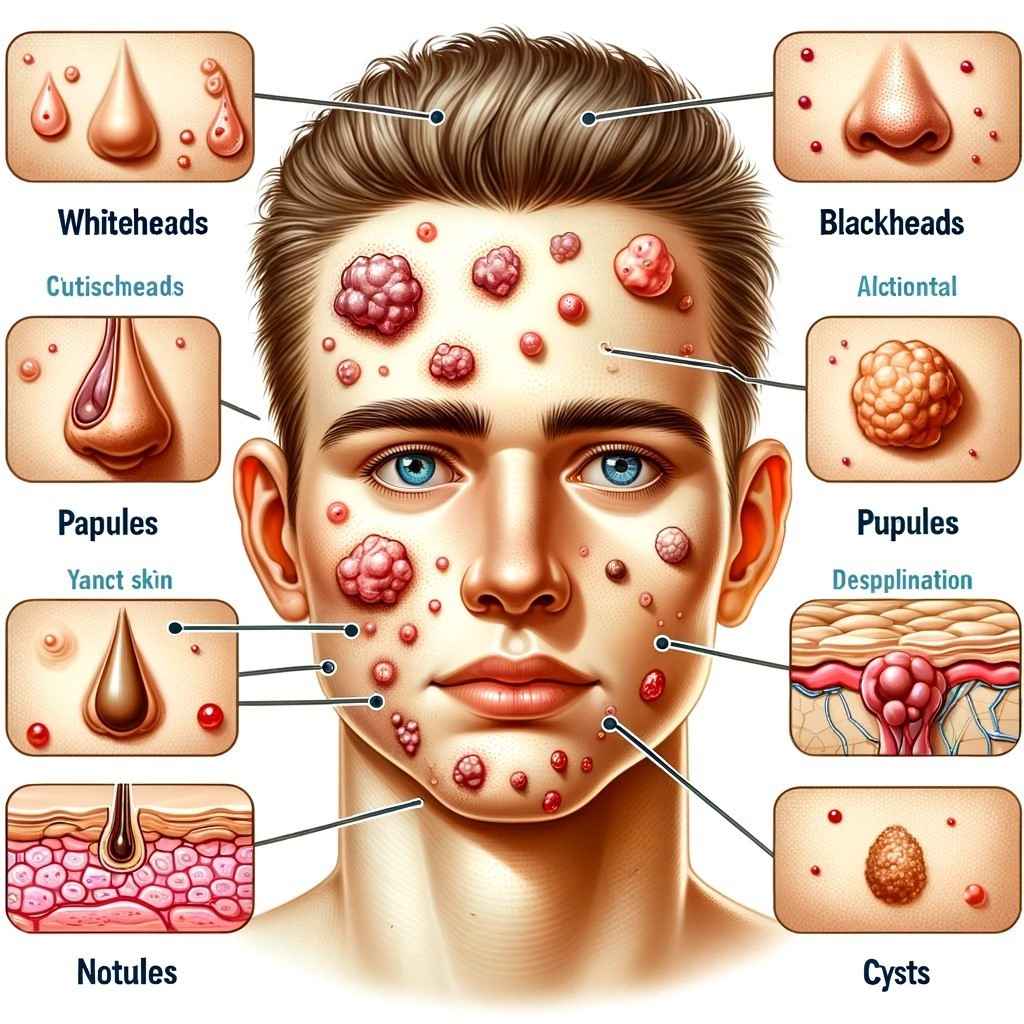
Acne is a common skin condition characterized by the clogging of hair follicles with oil and dead skin cells. It often leads to the formation of various types of skin lesions, including whiteheads, blackheads, papules, pustules, nodules, and cysts. Acne primarily affects the face but can appear on other parts of the body. It is most prevalent during adolescence due to hormonal changes but can affect individuals of all ages. Treatment options range from over-the-counter products to prescription medications and dermatological procedures, with the choice of treatment depending on the severity and type of acne.
Symptoms & Types of Acne
Certainly! Here are detailed symptoms of acne:
1.Comedones (Non-inflammatory Acne):
- Whiteheads (Closed Comedones):These are small, flesh-colored or white bumps on the skin’s surface. They occur when hair follicles become clogged with oil and skin cells but remain closed.
- Blackheads (Open Comedones): Blackheads are similar to whiteheads but have a dark or black appearance. They form when the pore is clogged and open to the air, causing the contents to oxidize and darken.
2.Inflammatory Acne:
- Papules: Papules are small, raised, red or pink bumps on the skin. They may be tender to the touch and often indicate an inflammatory response within the hair follicle.
- Pustules: Pustules are similar to papules but have a white or yellow center filled with pus. They can be painful and appear as visible, pus-filled pimples.
3.Nodules:
- Nodules are larger, solid, painful lumps beneath the surface of the skin. They form when clogged pores cause a deep inflammation reaction in the hair follicle. Nodules can be very painful and often lead to scarring.
4.Cysts:
- Cysts are the most severe form of acne lesions. They are large, painful, pus-filled lumps that can extend deep into the skin layers. Cysts are more likely to cause scarring and can be particularly distressing.
5.Redness and Inflammation:
- Acne-prone areas often appear red and inflamed due to the body’s immune response to the infection within the hair follicles.
6.Scarring:
- Severe acne, especially cystic and nodular types, can lead to permanent scarring. These scars can be atrophic (depressed) or hypertrophic (raised) and may affect the skin’s texture and appearance.
7.Post-Inflammatory Hyperpigmentation (PIH):
- After an acne lesion heals, it can leave behind dark spots or pigmentation changes on the skin. This is known as post-inflammatory hyperpigmentation and can persist for weeks or months.
8.Tenderness and Pain:
- Inflammatory acne lesions, such as papules, pustules, nodules, and cysts, are often painful and tender to the touch.
It’s important to note that acne symptoms can vary in severity from person to person. While some individuals may only experience mild whiteheads and blackheads, others may suffer from more severe and painful forms of acne. Proper diagnosis and treatment by a healthcare provider or dermatologist are essential to effectively manage acne and reduce the risk of scarring.
What are types of Acne?
Acne comes in several types, each with its own characteristics and features. Here’s a detailed overview of the main types of acne:
1.Acne Vulgaris:

Acne vulgaris, commonly referred to as acne, is a chronic skin condition that primarily affects the hair follicles and oil glands in the skin. It is characterized by the formation of various types of skin lesions, including comedones (whiteheads and blackheads), papules, pustules, nodules, and cysts.
2.Comedonal Acne:
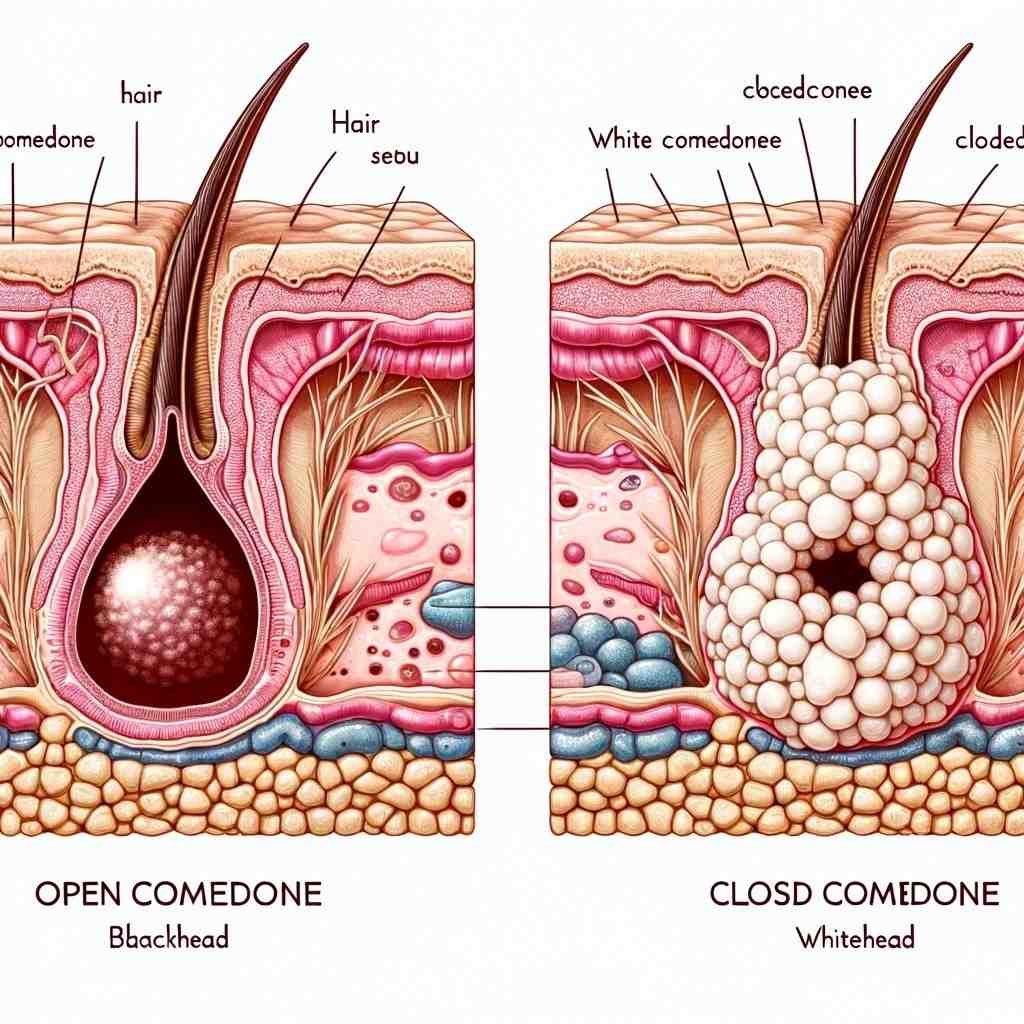
A comedo, which is the fundamental type of acne lesion, occurs when a hair follicle becomes obstructed by a combination of excess oil and dead skin cells. These comedones can progress into raised bumps known as whiteheads or blackheads. Substances that have the potential to provoke the formation of comedones are referred to as “comedogenic.” On the other hand, cosmetics labeled as “noncomedogenic” are less likely to block pores and exacerbate acne-related issues.
- Whiteheads (Closed Comedones): These are small, flesh-colored or white bumps with a closed surface. They form when hair follicles become clogged with oil and skin cells, trapping them beneath the skin’s surface.
- Blackheads (Open Comedones): Blackheads are similar to whiteheads but have a dark or black appearance. They develop when the clogged pore is open to the air, causing the contents to oxidize and turn black.
3.Inflammatory Acne:
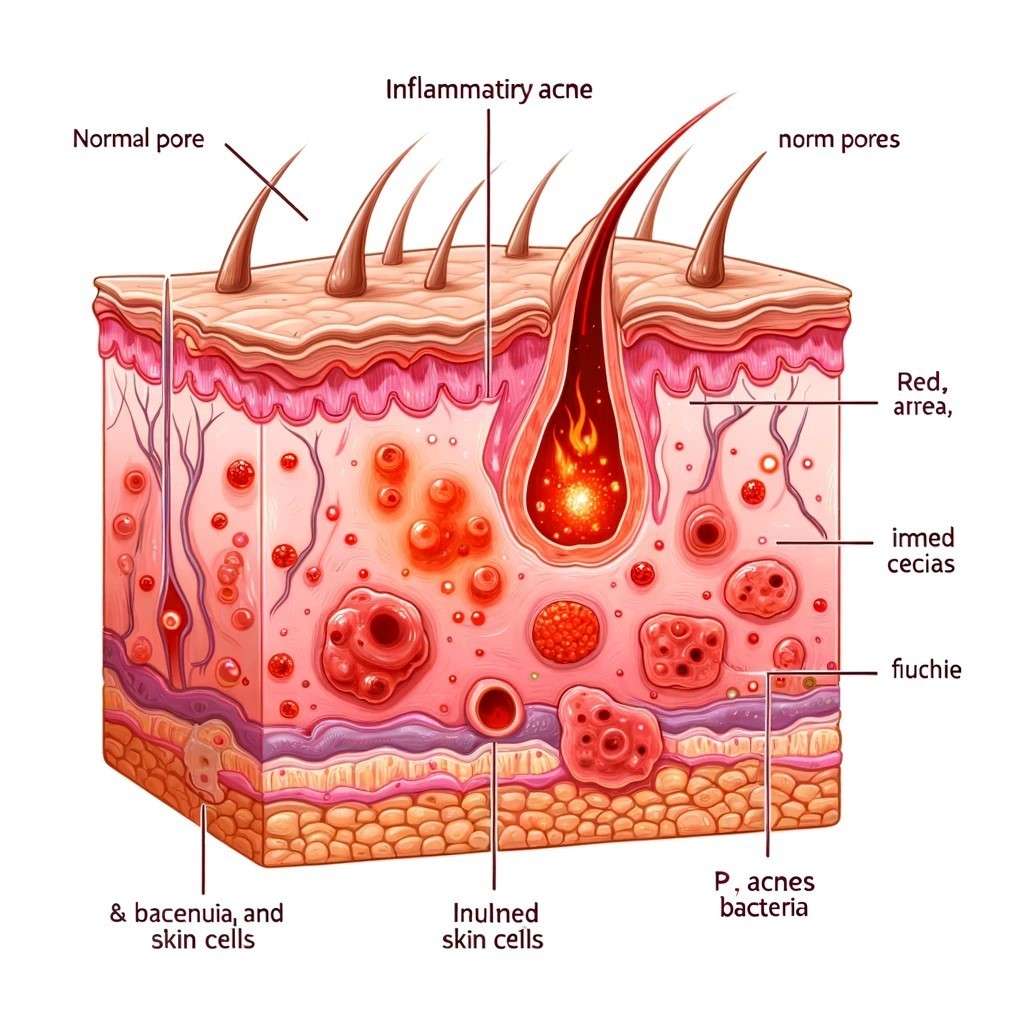
Inflamed acne is when pores get really red and swollen because they’re filled with oil, dead skin, and germs. A type of bacteria called Propionibacterium acnes, or P. acnes for short, can make this kind of acne worse.
- Papules: Papules are small, raised, red or pink bumps on the skin’s surface. They are often tender to the touch and result from inflammation within the hair follicle.
- Pustules: Pustules are also small, raised bumps, but they have a white or yellow center filled with pus. They are typically red at the base and appear as visible, pus-filled pimples.
4.Nodular Acne:

- Nodular acne is a more serious and painful type of acne that many people experience. It’s different because it causes big, hard lumps or nodules under the skin’s surface. These nodules form when hair follicles get really blocked up with oil, dead skin cells, and bacteria. This blockage triggers a strong and deep inflammation within the skin, which makes these lumps so painful and noticeable.
- Nodules acne is characterized by large, solid, painful lumps beneath the skin’s surface. These deep lesions develop due to severe inflammation within the hair follicle. Nodules can be particularly painful and often lead to scarring.
5.Cystic Acne:
- Cystic acne is an advanced and severe form of acne characterized by the formation of large, painful, deep-seated cysts or nodules beneath the skin’s surface. These cysts are filled with pus and can be associated with inflammation and tenderness. Cystic acne typically results from the same factors that cause other types of acne, including the blockage of hair follicles by excess oil, dead skin cells, and bacteria.
- Cysts: Cystic acne is the most severe form of acne. It involves large, painful, pus-filled lumps that extend deep into the skin layers. Cysts are highly inflammatory and can cause significant scarring if not treated
6.Acne Conglobata:
This is an extremely severe and rare form of acne that often affects males. It is characterized by deep, interconnected nodules and abscesses. Scarring is extensive in cases of acne conglobata.
7.Acne Fulminans:
Acne fulminans is a rare and severe type of acne that often occurs suddenly and is accompanied by systemic symptoms like fever and joint pain. It can result in significant scarring and requires prompt medical attention.
8.Acne Mechanica:
This type of acne is triggered by friction, pressure, or heat applied to the skin. It is common in athletes who wear helmets or tight clothing, and it typically appears in areas of repeated irritation.
9.Hormonal Acne:
Hormonal acne is often related to hormonal fluctuations, especially in females. It typically manifests as deep, tender cysts around the jawline and chin. It can be exacerbated during menstruation or due to conditions like polycystic ovary syndrome (PCOS).
10.Acne Rosacea:
Acne rosacea is a chronic skin condition that primarily affects the face. It can cause redness, visible blood vessels, and small, red bumps that resemble acne. However, it is a distinct condition from traditional acne.
11.Acne Excoriée:
This is a compulsive skin-picking disorder where individuals habitually pick, scratch, or squeeze their acne lesions, often leading to more severe inflammation and scarring.
It’s important to note that the severity and type of acne can vary from person to person, and proper diagnosis and treatment by a healthcare provider or dermatologist are crucial for effective management and prevention of scarring. Treatment options may include topical medications, oral medications, lifestyle changes, and dermatological procedures tailored to the specific type and severity of acne.
How acne, pimples & breakouts are different?
Acne:
- Definition: Acne is a common skin issue that shows up as different types of spots on your skin. These spots can include blackheads, whiteheads, red bumps, pus-filled pimples, big painful lumps, and deep nodules. Acne usually appears on your face, neck, chest, and back.
- Description: Acne happens when a mix of things goes wrong with your skin. Your skin makes too much oil, your pores get clogged with dead skin cells, and bad bacteria can make things worse. This can lead to pimples and other kinds of acne spots.
- Acne can be mild, where you might get a few small spots now and then, or it can be severe, with lots of painful and big lumps or nodules.
Pimple:
- Definition: A pimple, also called a zit or spot, is a single bump on your skin. It’s a type of blemish that forms when a tiny hair hole on your skin gets blocked with oil, dead skin cells, and germs.
- Description: Pimples usually look like raised red or pink bumps on your skin. Some might have a white or yellow top filled with pus. They can be sore and hurt a bit.
Breakout:
- Definition: A breakout is when you suddenly get a bunch of pimples or other blemishes on your skin, often happening all at once. It’s like your skin is having a bad day.
- Description: Breakouts can pop up for many reasons. It could be because of hormones changing, stress, the food you eat, or even the skincare products you use.
- What It Looks Like: During a breakout, you’ll see a bunch of pimples, blackheads, whiteheads, or other acne spots showing up together. They might appear on your face, and sometimes on other body parts, too.
Differences:
- Acne vs. Pimple: Acne is the bigger picture, including all kinds of skin spots like pimples. A pimple is just one type of acne spot, and it’s the one you can see on your skin’s surface.
- Pimple vs. Breakout: A pimple is that single bump that’s formed when your hair hole gets blocked. A breakout, on the other hand, is when you have several pimples or other blemishes appearing together, like a group of friends showing up at once.
- Acne vs. Breakout: Acne is the ongoing skin issue with various spots, while a breakout is a temporary event when your skin suddenly decides to have multiple pimples or other acne blemishes all at once.
- In summary, think of acne as the whole story of skin issues, pimples as individual bumps, and a breakout as the day when lots of those bumps appear together. It’s important to remember that breakouts are temporary, but acne might stick around for a while. Taking care of your skin can help manage both pimples and acne.
What are acne causing factors of Acne?
Acne is a multifactorial skin condition, meaning that it can be influenced by a combination of various factors. The exact cause of acne can vary from person to person, and several factors contribute to its development. Here are some of the key factors known to cause or exacerbate acne:
- Hormonal Changes: Hormonal fluctuations are a major contributor to acne, particularly during puberty, menstruation, pregnancy, and menopause. Hormones like androgens (e.g., testosterone) can stimulate increased sebum (skin oil) production, which can clog pores and lead to acne.
- Excess Sebum Production: An overproduction of sebum by the skin’s oil glands can increase the risk of developing acne. Sebum is necessary for healthy skin but can become problematic when produced in excess.
- Clogged Hair Follicles: Acne occurs when hair follicles become clogged with a combination of excess sebum, dead skin cells, and sometimes bacteria. This creates an ideal environment for acne to develop.
- Bacterial Growth: The presence of the acne-causing bacteria Propionibacterium acnes (P. acnes) within clogged follicles can exacerbate inflammation and contribute to the development of inflammatory acne lesions.
- Genetics: A family history of acne can increase an individual’s susceptibility to the condition. Genetics can influence how the skin produces sebum and responds to hormonal changes.
- Diet: Although the relationship between diet and acne is complex, certain foods and dietary factors may contribute to acne in some individuals. High-glycemic-index foods, dairy products, and diets rich in sugars and processed foods have been associated with acne in some studies.
- Stress: High stress levels can trigger hormonal changes that may worsen or exacerbate existing acne.
- Skincare Products: The use of certain skincare products or cosmetics that are comedogenic (pore-clogging) can contribute to acne breakouts.
- Medications: Some medications, including certain birth control pills, steroids, and drugs containing lithium, can increase the risk of acne as a side effect.
- Environmental Factors: Exposure to environmental pollutants, such as airborne particulates and chemicals, can contribute to skin inflammation and acne development, especially in individuals with sensitive skin.
- Pressure and Friction: Constant pressure or friction on the skin, as seen in helmet-wearing athletes or individuals who frequently wear tight clothing, can lead to a type of acne known as “acne mechanica.”
It’s important to note that the specific combination of factors contributing to acne can vary widely among individuals. Effective acne management often involves identifying and addressing these factors through lifestyle modifications, proper skincare, and, in some cases, medical treatments prescribed by a healthcare provider or dermatologist. Tailored treatment plans can help control and minimize the impact of acne on the skin.
Why do pimples form?
Pimples form when hair follicles become clogged with a combination of excess oil (sebum), dead skin cells, and bacteria, leading to inflammation and the development of a raised bump on the skin’s surface.
How do I know what triggers my acne?
Identifying the specific triggers for your acne can be a bit of a trial-and-error process, as acne can have multiple causes and triggers that vary from person to person. Here’s a step-by-step approach to help you pinpoint potential triggers for your acne:
- Keep a Skin Diary:
• Start by keeping a journal of your daily activities, skincare routine, diet, and any noticeable changes in your acne.
• Note when new breakouts occur and any potential factors that might be related. - Assess Your Skincare Routine:
• Examine the products you use on your skin, including cleansers, moisturizers, and makeup.
• Check for common acne-triggering ingredients like fragrances, comedogenic (pore-clogging) ingredients, or harsh exfoliants. - Dietary Factors:
• Pay attention to your diet. Some individuals find that certain foods, like dairy, high-sugar foods, or greasy items, can trigger acne.
• Experiment with dietary changes, such as reducing or eliminating specific foods, to see if it affects your skin. - Hormonal Influences:
• Consider hormonal factors. Hormonal fluctuations, especially in women, can play a significant role in acne.
• Track your menstrual cycle and hormonal changes, and discuss these patterns with a healthcare provider. - Stress Levels:
• Evaluate your stress levels. High stress can exacerbate acne for some individuals.
• Explore stress-reduction techniques like exercise, meditation, yoga, or deep breathing exercises. - Environmental Factors:
• Take note of environmental factors that could affect your skin, such as humidity, pollution, or exposure to harsh weather conditions.
• Adjust your skincare routine accordingly. - Medications and Supplements:
• Review any medications or supplements you are taking. Some medications or supplements can cause or worsen acne as a side effect.
• Discuss with your healthcare provider whether alternatives are available. - Allergens and Irritants:
• Consider allergens and irritants in your environment, such as certain fabrics or chemicals.
• Opt for hypoallergenic and non-comedogenic products. - Consult a Dermatologist:
• If you’re unable to identify the triggers on your own or your acne is persistent and severe, consult a dermatologist.
• Dermatologists can perform tests, prescribe appropriate treatments, and offer personalized guidance based on your skin’s needs. - Give It Time:
• Be patient. Identifying triggers may take time and experimentation.
• Make one change at a time, so you can better pinpoint the specific cause if your acne improves or worsens.
Remember that what triggers acne for one person may not be the same for another. Your unique skin type, genetics, and lifestyle factors all play a role. By carefully observing your skin and habits, you can gradually uncover the factors that contribute to your acne and make informed adjustments to your skincare routine and lifestyle.
Diagnosis of Acne
How acne can be diagnosed?
Acne is typically diagnosed through a visual examination of the skin by a healthcare provider or dermatologist. The diagnosis process involves assessing the type, severity, and distribution of acne lesions on the skin. Here are the key steps involved in diagnosing acne:
- Patient History: The healthcare provider will begin by taking a detailed medical history, including questions about the onset of acne, any family history of acne, and any factors that may exacerbate or improve the condition, such as diet, skincare routines, and medications.
- Physical Examination: The healthcare provider will visually inspect the affected areas of the skin, looking for various types of acne lesions, including whiteheads, blackheads, papules, pustules, nodules, and cysts. They will also assess the distribution and severity of the acne.
- Assessment of Lesions: The healthcare provider may gently press on the lesions to evaluate their tenderness and consistency. This helps determine if the acne is non-inflammatory or inflammatory in nature.
- Rule Out Other Conditions: In some cases, the healthcare provider may need to rule out other skin conditions that may mimic acne, such as rosacea or folliculitis.
- Severity Grading: In some instances, the healthcare provider may use a standardized grading system, such as the Global Acne Grading System (GAGS) or the Leeds Revised Acne Grading System, to assess the severity of the acne. This helps in determining the appropriate treatment approach.
- Evaluation of Contributing Factors: The provider may inquire about and evaluate factors that could be contributing to the acne, such as hormonal imbalances, medication use, or exposure to environmental irritants.
In some cases, if there is a suspicion of an underlying hormonal issue contributing to the acne, additional tests such as blood tests or hormonal assays may be ordered to assess hormonal levels.
It’s essential to consult with a healthcare provider or dermatologist for an accurate diagnosis and personalized treatment plan for acne. Early diagnosis and appropriate management can help prevent scarring and achieve clearer skin.
How do I know what type of acne I have?
- Non-Inflammatory Acne:
• Whiteheads (Closed Comedones): Small, flesh-colored bumps with a white center.
• Blackheads (Open Comedones): Small, dark spots with an open pore at the surface.
• Milia: Tiny, hard white bumps that are often seen around the eyes. - Inflammatory Acne:
• Papules: Small, red, tender bumps without a visible center.
• Pustules: Red, inflamed bumps with a white or yellow center of pus.
• Nodules: Large, painful, deep lumps beneath the skin’s surface.
• Cysts: Large, pus-filled lumps that are also deep and painful. - Hormonal Acne:
• Typically occurs along the jawline, chin, and lower face.
• May worsen in response to hormonal fluctuations, such as during menstruation. - Comedonal Acne:
• Characterized by the presence of whiteheads and blackheads.
• Often seen on the forehead, nose, and chin (T-zone). - Cystic Acne:
• Features large, painful cysts and nodules.
• Tends to be deep and can result in scarring.
• Typically requires medical intervention. - Back and Body Acne:
• Acne that appears on the chest, back, shoulders, and buttocks.
• May include whiteheads, blackheads, papules, pustules, and cysts.
Keep in mind that it’s not uncommon to have a combination of different acne types on your skin. To get a precise diagnosis and personalized treatment recommendations, it’s advisable to consult a healthcare provider or dermatologist. They can assess your skin and help you develop an effective acne management plan.
What are risk factors for developing acne?
Several risk factors can increase an individual’s likelihood of developing acne. It’s important to note that while these factors can contribute to acne development, they don’t guarantee that acne will occur. Acne is a complex skin condition influenced by multiple factors. Common risk factors for developing acne include
- Hormonal Changes: Hormonal fluctuations are a significant risk factor for acne. This includes changes during puberty, menstruation, pregnancy, and menopause. Hormones like androgens (e.g., testosterone) can stimulate sebum (skin oil) production, which can contribute to acne.
- Family History: A family history of acne can increase an individual’s susceptibility to the condition. Genetics can influence how the skin produces sebum and responds to hormonal changes.
- Age: Acne is most common during adolescence and early adulthood, but it can affect people of all ages. Teenagers are particularly susceptible due to hormonal changes during puberty.
- Gender: While acne affects both males and females, males may experience more severe and longer-lasting forms of acne. Hormonal fluctuations associated with the menstrual cycle can also contribute to acne in females.
- Cosmetic and Skincare Products: The use of certain makeup, skincare products, or hair products that are comedogenic (pore-clogging) can increase the risk of acne, especially if they are not properly removed.
- Diet: Some studies suggest that a high-glycemic diet (rich in sugars and refined carbohydrates) and dairy products may influence the development of acne in some individuals. However, the relationship between diet and acne is complex and varies from person to person.
- Stress: High levels of stress can trigger hormonal changes that may exacerbate or worsen existing acne.
- Exposure to Environmental Factors: Exposure to environmental pollutants, airborne particulates, and chemicals can contribute to skin inflammation and acne development, particularly in individuals with sensitive skin.
- Pressure and Friction: Constant pressure or friction on the skin, as seen in athletes who wear helmets or individuals who wear tight clothing, can lead to a type of acne known as “acne mechanica.”
- Medications: Some medications, including certain birth control pills, steroids, and drugs containing lithium, can have acne as a side effect.
- Comedogenic Products: The use of comedogenic skincare or haircare products can increase the risk of acne breakouts.
- Gut Health: Emerging research suggests that gut health and the microbiome may play a role in acne development, with imbalances potentially contributing to skin issues.
It’s important to recognize that acne is a common skin condition that can be managed with various treatments and lifestyle modifications. If you have concerns about acne or are experiencing persistent or severe breakouts, consider consulting a healthcare provider or dermatologist who can provide guidance and personalized treatment options. Early intervention can help prevent scarring and minimize the impact of acne on the skin.
Treatment of Acne
What are treatments of Acne?
The treatment of acne varies depending on its type, severity, and the individual’s specific needs. Treatment options can include over-the-counter products, prescription medications, and dermatological procedures. Here is an overview of common acne treatments:
- Topical Over-the-Counter (OTC) Products:
• Benzoyl Peroxide: Available in various strengths, benzoyl peroxide helps kill acne-causing bacteria, reduce inflammation, and unclog pores. It’s found in cleansers, lotions, and gels.
• Salicylic Acid: Salicylic acid helps exfoliate the skin, unclog pores, and reduce inflammation. It’s commonly found in acne cleansers, toners, and spot treatments.
• Alpha Hydroxy Acids (AHAs): AHAs like glycolic acid and lactic acid can help exfoliate the skin’s surface, improve texture, and reduce the appearance of blemishes. - Prescription Topical Medications:
• Topical Antibiotics: Antibiotic creams or gels, such as clindamycin or erythromycin, can help reduce acne-causing bacteria and inflammation.
• Retinoids: Prescription retinoid creams or gels like tretinoin, adapalene, and tazarotene help unclog pores, promote skin cell turnover, and reduce the formation of new comedones. - Oral Medications:
• Oral Antibiotics: Antibiotics like doxycycline, minocycline, or tetracycline may be prescribed to reduce inflammation and bacteria. They are typically used for moderate to severe acne.
• Hormonal Therapy: For individuals with hormonal acne, oral contraceptives (birth control pills) or anti-androgen medications may be recommended to regulate hormones.
• Isotretinoin (Accutane): Isotretinoin is a potent oral medication reserved for severe, resistant, or cystic acne. It works by reducing sebum production, shrinking oil glands, and preventing new comedone formation. It requires strict monitoring due to potential side effects. - Dermatological Procedures:
• Extraction: Dermatologists can perform manual extraction of comedones (blackheads and whiteheads) using specialized tools.
• Chemical Peels: Chemical peels containing acids like salicylic acid, glycolic acid, or trichloroacetic acid can improve skin texture and reduce acne.
• Laser and Light Therapies: Various laser and light-based treatments, such as photodynamic therapy (PDT) or intense pulsed light (IPL), can target acne-causing bacteria and reduce inflammation.
• Corticosteroid Injections: Intralesional corticosteroid injections are used to treat large, painful cysts or nodules by reducing inflammation and discomfort. - Lifestyle and Skincare Modifications:
• Proper Cleansing: Gently cleanse the skin with a mild, non-comedogenic cleanser.
• Avoiding Irritants: Avoid skincare products that may irritate the skin, and refrain from picking or squeezing acne lesions.
• Sun Protection: Use sunscreen daily to prevent post-inflammatory hyperpigmentation and protect the skin from sun damage.
• Diet and Lifestyle: Maintain a healthy diet, manage stress, and get regular exercise, as these factors can impact acne.
Treatment plans are often individualized, and it may take several weeks or months to see significant improvement. It’s essential to work with a healthcare provider or dermatologist to determine the most appropriate treatment for your specific type and severity of acne and to monitor progress effectively.
What medications are used for Acne?
Several medications are commonly used to treat acne, ranging from over-the-counter (OTC) options to prescription medications. The choice of medication depends on the type and severity of acne, as well as individual factors. Here are some safe and effective medications for acne:
- Over-the-Counter (OTC) Topical Products:
• Benzoyl Peroxide: Available in various strengths (2.5%, 5%, or 10%), benzoyl peroxide is an effective OTC ingredient that helps kill acne-causing bacteria, reduce inflammation, and unclog pores. It’s available in various forms, including gels, creams, and washes.
• Salicylic Acid: Salicylic acid is an OTC topical treatment that helps exfoliate the skin, unclog pores, and reduce inflammation. It’s commonly found in acne cleansers, toners, and spot treatments.
• Alpha Hydroxy Acids (AHAs): AHAs like glycolic acid and lactic acid can help exfoliate the skin’s surface, improve texture, and reduce the appearance of blemishes. - Prescription Topical Medications:
• Topical Antibiotics: Antibiotic creams or gels, such as clindamycin or erythromycin, are prescribed to reduce acne-causing bacteria and inflammation. They are typically used for mild to moderate acne.
• Retinoids: Prescription retinoid creams or gels like tretinoin, adapalene, and tazarotene help unclog pores, promote skin cell turnover, and reduce the formation of new comedones. They are effective for various types of acne and are often used in combination with other treatments. - Oral Medications:
• Oral Antibiotics: Antibiotics like doxycycline, minocycline, or tetracycline may be prescribed to reduce inflammation and bacteria. They are typically used for moderate to severe acne but are not recommended for long-term use due to concerns about antibiotic resistance.
• Hormonal Therapy: For individuals with hormonal acne, oral contraceptives (birth control pills) or anti-androgen medications like spironolactone may be recommended to regulate hormones and reduce sebum production.
• Isotretinoin (Accutane): Isotretinoin is a potent oral medication reserved for severe, resistant, or cystic acne. It works by reducing sebum production, shrinking oil glands, and preventing new comedone formation. It requires strict monitoring due to potential side effects and must be prescribed by a dermatologist. - Oral Contraceptives: Some oral contraceptives with anti-androgen properties may be prescribed to regulate hormones and improve hormonal acne in females.
- Corticosteroid Injections: Dermatologists may inject corticosteroids directly into large, painful cysts or nodules to reduce inflammation and discomfort.
- Laser and Light Therapies: Various laser and light-based treatments, such as photodynamic therapy (PDT) or intense pulsed light (IPL), can be used in dermatology clinics to target acne-causing bacteria and reduce inflammation.
The choice of medication and treatment plan should be determined by a healthcare provider or dermatologist based on the type and severity of acne, as well as individual factors like age, gender, and medical history. They can help you select the safest and most effective treatment for your specific acne condition while monitoring and managing any potential side effects.
Which medications have best results for acne?
The choice of medications for acne depends on the type, severity, and individual characteristics of the condition. What works best for one person may not be as effective for another. However, some medications and treatments have consistently shown good results for acne management when prescribed and used correctly. Here are several medications and treatment options that are often considered effective for acne:
- Topical Retinoids:
• Tretinoin (Retin-A): Tretinoin is a potent topical retinoid that helps unclog pores, increase skin cell turnover, and reduce the formation of new comedones. It is effective for various types of acne, including blackheads and whiteheads.
• Adapalene (Differin): Adapalene is another topical retinoid available over-the-counter and by prescription. It works similarly to tretinoin in treating acne and is suitable for mild to moderate cases. - Topical Antibiotics:
• Clindamycin and Erythromycin: These topical antibiotics can reduce inflammation and the growth of acne-causing bacteria. They are often prescribed for mild to moderate inflammatory acne. - Benzoyl Peroxide:
• Benzoyl peroxide is available in various strengths and forms (gels, creams, washes). It helps kill acne-causing bacteria, reduce inflammation, and unclog pores. It is suitable for various types of acne and is often used as a first-line treatment. - Oral Antibiotics:
• Doxycycline, Minocycline, Tetracycline: Oral antibiotics can be effective for moderate to severe inflammatory acne. They help reduce inflammation and the growth of acne-causing bacteria. However, long-term use is discouraged due to concerns about antibiotic resistance. - Hormonal Therapy:
• Oral Contraceptives (Birth Control Pills): Certain birth control pills can help regulate hormones and reduce sebum production, making them effective for hormonal acne in females.
• Spironolactone: Spironolactone is an anti-androgen medication that can be used to manage hormonal acne in females. It helps reduce the effects of androgens, which can contribute to acne. - Isotretinoin (Accutane):
• Isotretinoin is a potent oral medication reserved for severe, resistant, or cystic acne. It is highly effective but requires strict medical supervision due to potential side effects. It works by reducing sebum production, shrinking oil glands, and preventing new comedone formation. - Chemical Peels:
• Chemical peels containing acids like salicylic acid, glycolic acid, or trichloroacetic acid can improve skin texture, reduce acne lesions, and promote skin renewal when performed by a dermatologist. - Laser and Light Therapies:
• Various laser and light-based treatments, such as photodynamic therapy (PDT) and intense pulsed light (IPL), can target acne-causing bacteria, reduce inflammation, and improve skin texture. - Corticosteroid Injections:
• Dermatologists may inject corticosteroids directly into large, painful cysts or nodules to reduce inflammation and discomfort.
The effectiveness of these treatments can vary from person to person, and a healthcare provider or dermatologist can help determine the most suitable approach based on your specific acne type and severity. It’s important to follow the prescribed treatment plan, maintain proper skincare, and attend follow-up appointments to monitor progress and manage any potential side effects.
What are natural treatments for acne?
Natural treatments for acne can be a complementary or alternative approach to managing mild to moderate acne. Keep in mind that while these remedies may help improve skin health, they may not be as effective as prescription or medical treatments for severe acne. Here are some natural treatments and home remedies for acne:
- Tea Tree Oil: Tea tree oil has natural antibacterial and anti-inflammatory properties. Diluted tea tree oil can be applied topically to acne-prone areas as a spot treatment. Be cautious not to use it undiluted, as it can be irritating to the skin.
- Honey: Honey has antibacterial and wound-healing properties. Applying a thin layer of honey to acne lesions and leaving it on for about 15-20 minutes before rinsing off can help soothe and reduce inflammation.
- Aloe Vera: Aloe vera gel can be applied to acne-prone areas to reduce redness and inflammation. It’s moisturizing and can help with healing skin.
- Apple Cider Vinegar: Diluted apple cider vinegar (1 part vinegar to 3-4 parts water) can be used as a toner. Apply it to the skin with a cotton ball, leave it on for a few minutes, and then rinse off. It may help balance the skin’s pH and reduce the growth of acne-causing bacteria.
- Green Tea Extract: Green tea contains antioxidants that can help reduce inflammation. Applying cooled green tea as a toner or using skincare products with green tea extract may be beneficial.
- Zinc Supplements: Zinc is an essential mineral for skin health. Some people with acne have lower zinc levels. Taking zinc supplements as directed by a healthcare provider can help improve skin condition.
- Dietary Modifications: Some individuals find that reducing dairy consumption, avoiding high-glycemic foods (sugars and refined carbohydrates), and incorporating more fruits, vegetables, and omega-3 fatty acids into their diet can improve their skin.
- Probiotics: Probiotic supplements or foods with probiotics (like yogurt or kefir) may help balance gut bacteria, potentially improving skin health. Gut health is connected to skin health.
- Maintain Good Hygiene: Keeping your face clean by gently washing it twice a day with a mild, non-comedogenic cleanser can help prevent acne breakouts.
- Manage Stress: Stress can exacerbate acne. Engage in stress-reduction techniques such as meditation, yoga, or deep breathing exercises.
- Hydration: Drink plenty of water to keep the skin hydrated and support overall skin health.
Remember that not all natural remedies work for everyone, and individual responses can vary. It’s essential to be patient, as natural treatments may take time to show results. If you have severe or persistent acne, it’s advisable to consult a healthcare provider or dermatologist for a more comprehensive treatment plan. They can help determine the most effective approach for your specific acne type and severity.
What are home remedies for acne?
Natural home remedies for acne can be a helpful addition to your skincare routine for managing mild to moderate acne. While these remedies may not replace prescription medications for severe acne, they can contribute to clearer skin when used consistently. Here are some natural home remedies for acne:
- Tea Tree Oil: Tea tree oil has natural antibacterial and anti-inflammatory properties. Dilute a few drops of tea tree oil in a carrier oil (like jojoba or coconut oil) and apply it to acne-prone areas as a spot treatment. Be cautious not to use it undiluted, as it can be harsh on the skin.
- Honey: Honey has antibacterial and soothing properties. Apply a thin layer of honey to acne lesions and leave it on for about 15-20 minutes before rinsing off with warm water.
- Aloe Vera: Aloe vera gel can help reduce redness and inflammation. Apply pure aloe vera gel directly to acne-prone areas or use skincare products containing aloe vera.
- Apple Cider Vinegar: Diluted apple cider vinegar (1 part vinegar to 3-4 parts water) can be used as a toner. Apply it to the skin with a cotton ball, leave it on for a few minutes, and then rinse off. Be cautious if you have sensitive skin, as it can be drying.
- Green Tea: Green tea contains antioxidants and anti-inflammatory properties that may help reduce acne. Brew a cup of green tea, allow it to cool, and use it as a facial toner or in homemade face masks.
- Oatmeal: Oatmeal can soothe irritated skin and absorb excess oil. Mix cooked and cooled oatmeal with honey and apply it as a mask. Rinse off after 15-20 minutes.
- Turmeric: Turmeric has anti-inflammatory and antioxidant properties. Create a paste by mixing turmeric powder with water or yogurt and apply it to acne-prone areas for 10-15 minutes before rinsing.
- Cucumber: Cucumber slices or cucumber juice can help hydrate the skin and reduce redness and swelling. Apply cucumber slices or juice to affected areas.
- Baking Soda: Baking soda can be used as a gentle exfoliant. Mix a small amount with water to form a paste and apply it to the skin in a circular motion. Rinse off after a few minutes.
- Probiotics: Consuming probiotic-rich foods like yogurt and kefir or taking probiotic supplements may help support gut health, which can be linked to skin health.
- Maintain Good Hygiene: Keep your face clean by gently washing it twice a day with a mild, non-comedogenic cleanser.
- Hydration: Drinking plenty of water can help keep the skin hydrated and promote overall skin health.
Remember to be patient when using natural remedies, as they may take time to show results. If you have severe or persistent acne, consult with a healthcare provider or dermatologist for a more comprehensive treatment plan tailored to your specific needs. Additionally, perform a patch test before using any new natural remedy to check for potential skin sensitivity or allergies.
Which supplements are used to treat acne?
Certain dietary supplements may be used as complementary or adjunctive treatments for acne, particularly when there are underlying nutritional deficiencies or specific skin-related concerns. It’s essential to consult with a healthcare provider before taking any supplements to determine if they are appropriate for your individual needs. Here are some supplements that are sometimes used in the management of acne:
- Zinc: Zinc is an essential mineral for skin health. Some individuals with acne may have lower zinc levels. Zinc supplements, when taken as directed by a healthcare provider, may help reduce inflammation and support skin healing.
- Vitamin A: Vitamin A, specifically in the form of retinoids, is used in prescription medications for acne. However, excessive vitamin A intake can be toxic, so it’s important to use these supplements under medical supervision.
- Omega-3 Fatty Acids: Omega-3 fatty acids found in fish oil supplements have anti-inflammatory properties and may help reduce inflammation associated with acne. They are available as capsules or liquids.
- Probiotics: Probiotic supplements contain beneficial bacteria that can support gut health. Emerging research suggests a connection between gut health and skin health, and probiotics may be beneficial for some individuals with acne.
- Vitamin D: Adequate vitamin D levels are essential for overall health, including skin health. While vitamin D supplements are not a primary treatment for acne, ensuring you have sufficient vitamin D through diet, sun exposure, or supplements may support overall skin health.
- Niacinamide (Vitamin B3): Niacinamide is a form of vitamin B3 that is found in some skincare products. It may help improve the skin’s barrier function and reduce inflammation. It is often applied topically but is also available in oral supplements.
- Evening Primrose Oil: Evening primrose oil contains gamma-linolenic acid (GLA), an omega-6 fatty acid. Some individuals use GLA supplements to manage hormonal acne, but evidence for its effectiveness is limited.
- Selenium: Selenium is a trace mineral that acts as an antioxidant and may help reduce inflammation. Selenium supplements should be used under medical guidance, as excessive intake can be harmful.
It’s crucial to emphasize that supplements should not replace a balanced diet and should only be used under the guidance of a healthcare provider. Nutritional deficiencies can contribute to acne, but not all cases of acne are related to nutrient deficiencies. A healthcare provider can perform appropriate tests and assessments to determine if supplementation is necessary and can provide recommendations based on your specific needs. Additionally, excessive intake of certain supplements can be harmful, so it’s essential to follow recommended dosages and guidelines.
What is best treatment for pimples & acne?
When it comes to treating pimples and acne, the right approach depends on your unique situation. There isn’t a one-size-fits-all solution, but there are some general steps you can follow to help manage these skin issues.
- Skincare Routine:
- Gentle Cleansing: Use a mild face wash twice a day to clean your skin. Avoid harsh scrubbing, as it can make acne worse.
- Topical Products: Consider using over-the-counter acne products that contain ingredients like benzoyl peroxide, salicylic acid, or alpha hydroxy acids (such as glycolic or lactic acid). These ingredients can help unclog pores and reduce acne.
- Moisturize: Even if your skin is oily, use a non-comedogenic moisturizer to keep your skin hydrated without causing more pimples.
- Sun Protection: Apply sunscreen with SPF 30 or higher every day to protect your skin from the sun and prevent dark spots left behind by acne.
- Avoid Irritants: Be careful with abrasive scrubs, astringents, or products that contain alcohol because they can irritate your skin.
- Lifestyle Changes:
• Diet: While the connection between diet and acne varies from person to person, some people find that cutting back on sugary and refined foods and dairy products can help.
• Stress Management: High stress levels can make acne worse by affecting hormones. Try relaxation techniques like meditation, yoga, or deep breathing exercises.
• Hydration: Drinking enough water keeps your skin healthy and helps with acne management.
• Hands Off: Resist the urge to pick or pop your pimples. Doing so can lead to scarring and more inflammation. - Medications:
• If over-the-counter products aren’t doing the trick, see a healthcare provider or dermatologist. They may recommend prescription-strength topical medications, oral antibiotics, or hormonal treatments if your acne is related to hormones.
• For severe or stubborn acne, isotretinoin (Accutane) might be an option, but it comes with potential side effects and needs careful medical supervision. - Dermatological Procedures:
• Dermatologists can perform treatments like chemical peels, microdermabrasion, and extractions to target acne and improve your skin’s texture. - Consistency and Patience:
• Remember that acne treatment takes time, and you might not see immediate results. Stick to your skincare routine and follow your healthcare provider’s advice.
It’s important to work with a healthcare provider or dermatologist to figure out the best treatment plan for your specific acne. They can offer personalized guidance, track your progress, and make any necessary adjustments to help you achieve clearer skin while reducing the risk of scarring.
How can get rid of acne as quickly as possible?
Getting rid of acne quickly is a common goal, but it’s important to note that there is no instant or overnight solution for acne. Acne treatments usually take time to show significant results. However, here are some steps you can take to help manage and improve acne as quickly as possible:
- Start with a Gentle Cleanser:
Wash your face twice a day using a mild, skin-friendly cleanser. Avoid rubbing your skin too hard as it can make acne worse. - Try Over-the-Counter (OTC) Acne Products:
Look for OTC products that contain active ingredients like benzoyl peroxide, salicylic acid, or AHAs. These can help clear clogged pores and reduce acne. Follow the instructions on the product label. - Use Spot Treatments:
If you have individual pimples, use OTC spot treatments with ingredients like benzoyl peroxide or salicylic acid directly on the affected areas. Be careful not to use them excessively, as it can dry out your skin. - Keep Your Skin Moisturized:
Even if you have oily skin, use a moisturizer that won’t clog your pores. Moisturizing is important to maintain skin health. - Hands Off:
Avoid the temptation to pop or squeeze pimples. Doing so can lead to scarring and make matters worse. - Watch Your Diet and Stay Hydrated:
Consider reducing your intake of sugary and processed foods, as well as dairy products, as they may affect some people’s acne.
Drink plenty of water to keep your skin hydrated and healthy. - Manage Stress:
Practice stress-reduction techniques such as meditation, yoga, or deep breathing exercises. Stress can exacerbate acne. - Topical Retinoids (Prescription):
If your acne is more severe, consult a healthcare provider or dermatologist for prescription-strength treatments like tretinoin or adapalene. - Oral Medications (Prescription):
For severe acne, a healthcare provider may prescribe oral antibiotics, hormonal treatments (for hormonal acne in females), or isotretinoin (Accutane). Discuss the pros and cons with your healthcare provider. - Dermatological Procedures (Dermatologist):
Dermatologists can perform procedures like chemical peels, extractions, corticosteroid injections, or laser treatments to target acne and improve your skin’s texture. - Sun Protection:
Protect your skin from the sun by using sunscreen with SPF 30 or higher. Sun exposure can worsen acne and lead to dark spots. - Seek Professional Guidance:
If your acne persists, worsens, or is causing emotional distress, consult a healthcare provider or dermatologist. They can create a personalized treatment plan to address your specific needs.
Remember, consistent care is essential when dealing with acne. While you may not see instant results, sticking to a well-rounded skincare routine can help you get rid of acne as quickly as possible while reducing the risk of scarring.
What is most recommended face wash for acne?
The most recommended face wash for treating acne often contains ingredients that help to unclog pores, reduce excess oil, and manage acne-related concerns. However, the ideal face wash can vary depending on your skin type, the severity of your acne, and individual sensitivities. Here are some key ingredients and types of face washes that are commonly recommended for acne-prone skin:
- Salicylic Acid Face Wash:
- Recommended: If you have mild to moderate acne, including blackheads and whiteheads.
- How it works: Salicylic acid is like a key that unlocks your clogged pores. It helps get rid of excess oil, dead skin cells, and gunk inside your pores, which can prevent new pimples.
- Usage: Use it once or twice a day. Start with a lower concentration (around 0.5%) and go higher if your skin can handle it.
- Benzoyl Peroxide Face Wash:
Recommended: If your acne includes pimples and pustules.
How it works: Benzoyl peroxide is like a bouncer at a party, kicking out the acne-causing bacteria and calming down the redness and swelling.
Usage: Apply it once a day, and if your skin tolerates it well, you can bump it up to twice daily. Begin with a lower concentration (2.5%) to avoid irritation. - Gentle, Non-Comedogenic Face Wash:
Recommended: Sensitive skin or if you’re using other acne treatments that might be harsh on your skin.
How it works: This face wash is like a gentle friend for your skin. It cleans without causing dryness or irritation.
Usage: Use it twice a day, especially if you’re using other acne products. - Sulfur-Based Face Wash:
Recommended: Mild acne or if you prefer natural ingredients.
How it works: Sulfur is like a mini plumber for your pores. It helps clear out blockages, reduces oily skin, and has a gentle antibacterial effect.
Usage: Once a day or as your healthcare provider suggests. - Prescription Face Washes:
Recommended: If you have moderate to severe acne that isn’t getting better with OTC products.
How they work: These face washes contain stronger ingredients like antibiotics or special acne fighters, which need a doctor’s guidance.
Usage: Follow your healthcare provider’s instructions carefully.
Remember, patience is key. It might take a few weeks before you see noticeable changes in your skin. If you have sensitive skin or are using prescription treatments, it’s a good idea to chat with a healthcare provider or dermatologist to find the best face wash for your specific acne and skin type. They can give you personalized advice and keep an eye on how your skin is doing.
Can I clear up hormonal acne without taking medication for it?
Yes, it is possible to improve hormonal acne without taking medication, although the effectiveness of non-medication approaches may vary from person to person. Here are some strategies you can try:
- Skincare Routine: Establish a consistent skincare routine that includes gentle cleansing, exfoliation, and moisturizing. Choose products that are suitable for your skin type. Avoid harsh or abrasive scrubs that can irritate the skin.
- Topical Treatments: Over-the-counter topical treatments containing ingredients like benzoyl peroxide, salicylic acid, or alpha hydroxy acids (AHAs) can help manage mild hormonal acne by reducing inflammation and unclogging pores.
- Diet: Some people find that making dietary changes can help manage hormonal acne. Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Limit your intake of processed foods, sugary items, and dairy products, as these may contribute to acne for some individuals.
- Stress Management: High stress levels can trigger hormonal fluctuations that worsen acne. Practicing stress-reduction techniques such as yoga, meditation, deep breathing, or regular exercise may help.
- Hydration: Stay well-hydrated by drinking plenty of water. Proper hydration supports overall skin health.
- Clean Pillowcases and Bedding: Frequently change your pillowcases and sheets to prevent the buildup of oils, dirt, and bacteria that can contribute to acne.
- Non-comedogenic Products: Use makeup and skincare products labeled as “non-comedogenic” or “oil-free” to reduce the risk of clogged pores.
- Avoid Touching or Picking: Refrain from touching your face or picking at acne lesions, as this can worsen inflammation and lead to scarring.
- Regular Exercise: Engage in regular physical activity to help maintain hormonal balance and reduce stress. Be sure to cleanse your skin after exercising to remove sweat and dirt.
- Consult a Dermatologist: If your hormonal acne is severe, persistent, or causing significant distress, consider consulting a dermatologist. They can provide professional guidance, recommend appropriate treatments, and discuss prescription options if necessary.



