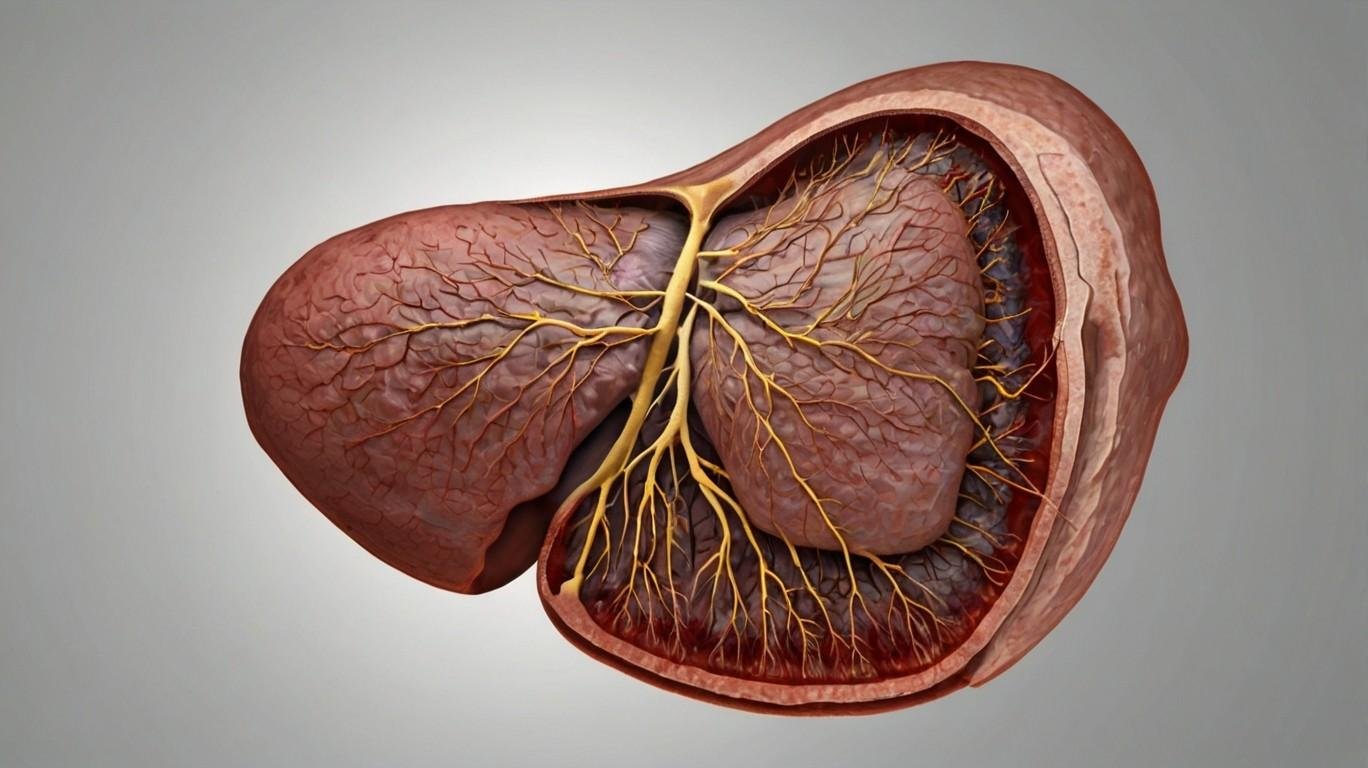
The liver, one of the body’s largest and most vital organs, plays an essential role in maintaining overall health. Among its many duties, the liver processes nutrients from the digestive system, detoxifies harmful substances, synthesizes proteins necessary for blood clotting, and produces bile, which aids in digestion. Additionally, the liver helps regulate blood sugar levels, stores vitamins and minerals, and metabolizes drugs and hormones. Its versatility and importance make it indispensable for survival.
Introduction / Statistics / Demographics / Types / Causes / Symptoms / Natural Remedies / Dietary / Treatment / tests / Liver Biopsy
Liver failure
Introduction
Liver failure occurs when the liver loses its ability to perform these essential functions, either suddenly or gradually. Liver failure can manifest in two primary forms: acute liver failure (ALF), which develops rapidly over days or weeks in individuals without pre-existing liver disease, and chronic liver failure, which progresses slowly over months or years, often due to long-term conditions like cirrhosis.
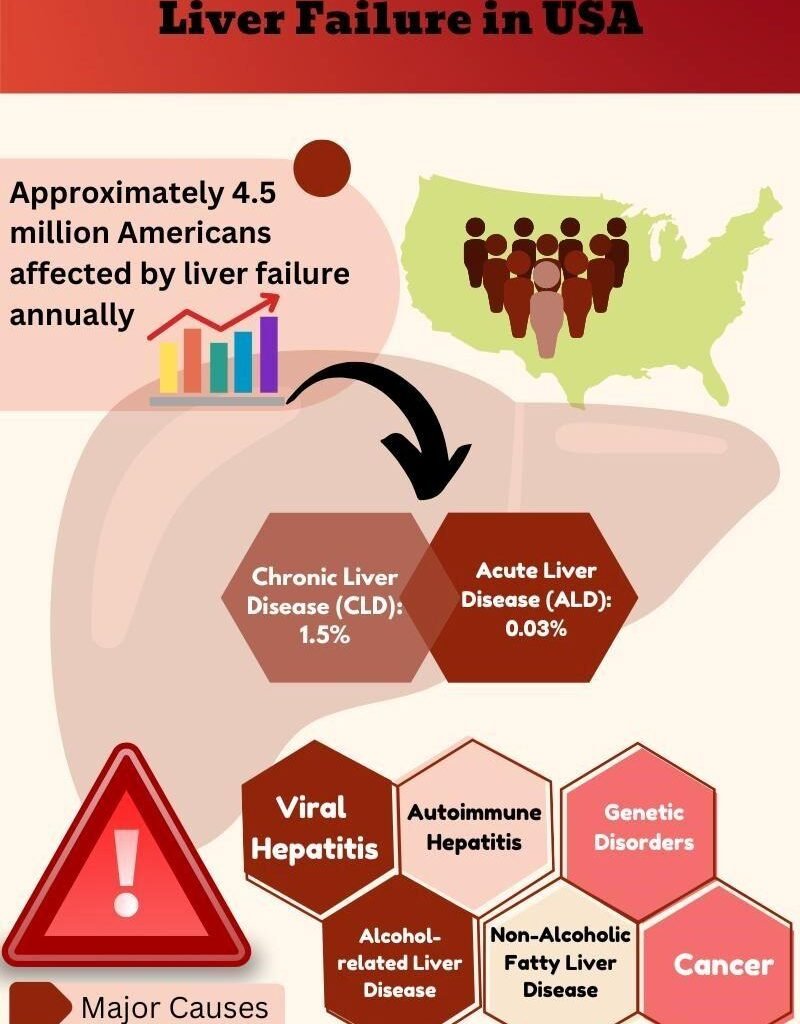
Prevalence and Statistics of liver failure
Liver failure is a global health concern, with both acute and chronic liver failure affecting millions of people worldwide. The prevalence varies significantly by region, demographic factors such as age, gender, and ethnicity, as well as underlying causes like alcohol consumption, viral hepatitis, and non-alcoholic fatty liver disease (NAFLD).
| Region | Prevalence of Liver Failure (2023) | Comments |
| Global | 2 million deaths annually | Chronic liver disease accounts for over 1 million deaths; acute liver failure responsible for additional deaths. |
| United States | 5.5 million people | Alcoholic liver disease and NAFLD are leading causes. |
| Europe | 29 million people affected | Significant burden due to alcohol-related liver diseases, particularly in Eastern Europe. |
| Asia | 32% of global liver failure cases | High prevalence of viral hepatitis (Hepatitis B and C). |
| Africa | 7-10% of population at risk | Limited healthcare access contributes to complications from hepatitis infections. |
| Latin America | 12-14% of adult population | Rising incidence of NAFLD due to increasing obesity rates. |
Demographics of Liver Failure
Understanding the demographic factors contributing to liver failure is crucial for developing targeted interventions and improving patient outcomes.
| Demographic Factor | Prevalence and Statistics | Comments |
| Age | 45-65 years: Highest incidence of chronic liver failure | Chronic liver failure typically results from long-term conditions like cirrhosis and NAFLD |
| Gender | Men: Higher risk (60-65% of cases) | Men are more prone to alcohol-related liver diseases. |
| Women: Increasing rates (especially due to NAFLD) | Non-alcoholic fatty liver disease is on the rise in women, driven by metabolic factors. | |
| Ethnicity | African Americans and Hispanics: Higher rates of liver failure | Disproportionately affected by metabolic syndrome and viral hepatitis. |
| Asian Populations: Higher prevalence of hepatitis B and C. | Chronic viral infections are a significant cause of liver disease. |
Types of Liver Failure
Liver failure is categorized into two main types: acute liver failure (ALF) and chronic liver failure. Each type has distinct causes, progression, and treatment approaches, yet both result in the inability of the liver to perform its essential functions. Understanding the differences between these two forms is critical for effective diagnosis, treatment, and management.
- Acute Liver Failure (ALF)
- Chronic Liver Failure
Acute Liver Failure (ALF)
Acute liver failure is a rare, life-threatening condition characterized by the rapid loss of liver function, typically within days or weeks. It occurs in individuals who previously had no known liver disease. The condition can lead to serious complications, including hepatic encephalopathy (brain dysfunction due to liver damage), coagulation abnormalities, and multi-organ failure.
Causes Of ALF
- Drug-Induced Liver Injury (DILI): Acetaminophen (paracetamol) overdose is the most common cause of ALF, especially in Western countries. Other drugs, such as antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and herbal supplements, can also cause liver toxicity.
- Viral Infections: Hepatitis A, B, and E can cause ALF, particularly in areas with limited healthcare access. Hepatitis B can also cause fulminant liver failure, a severe and rapid form of ALF.
- Toxins: Exposure to certain toxins, including poisonous mushrooms (e.g., Amanita phalloides) and industrial chemicals, can lead to ALF.
- Autoimmune Hepatitis: In some cases, the immune system mistakenly attacks liver cells, causing rapid inflammation and damage.
- Vascular Disorders: Conditions like Budd-Chiari syndrome, where blood flow out of the liver is obstructed, can cause ALF.
Chronic Liver Failure
Chronic liver failure develops gradually over months or years as the liver undergoes repeated damage, leading to fibrosis (scarring) and eventually cirrhosis. This progressive damage results in the liver’s inability to regenerate and function properly. Unlike ALF, chronic liver failure is usually the culmination of long-term liver diseases.
Causes
- Chronic Alcohol Abuse: Long-term excessive alcohol consumption is a leading cause of chronic liver failure, often leading to alcoholic liver disease (ALD) and cirrhosis.
- Non-Alcoholic Fatty Liver Disease (NAFLD): NAFLD is becoming a major cause of chronic liver failure globally, driven by rising rates of obesity, diabetes, and metabolic syndrome. In its more severe form, non-alcoholic steatohepatitis (NASH), it can lead to cirrhosis and liver failure.
- Viral Hepatitis (B and C): Chronic infection with hepatitis B or C can cause liver inflammation and scarring over time, leading to cirrhosis and liver failure. Hepatitis C, in particular, is a major contributor to liver disease worldwide.
- Autoimmune Liver Diseases: Autoimmune hepatitis, primary biliary cirrhosis (PBC), and primary sclerosing cholangitis (PSC) are autoimmune disorders that can lead to chronic liver failure due to long-term inflammation and damage.
- Genetic Conditions: Inherited disorders such as Wilson’s disease (copper buildup in the liver) and hemochromatosis (iron overload) can result in liver damage and eventual failure if untreated.
Difference Between Acute and Chronic Liver Failure
| Feature | Acute Liver Failure (ALF) | Chronic Liver Failure |
| Onset | Rapid (days to weeks) | Gradual (months to years) |
| Underlying Disease | No pre-existing liver disease | Often associated with long-term liver disease (e.g., cirrhosis) |
| Common Causes | Acetaminophen overdose, viral hepatitis | Alcohol abuse, NAFLD, hepatitis B and C |
| Symptoms | Sudden onset of jaundice, confusion, bleeding | Fatigue, jaundice, ascites, encephalopathy |
| Prognosis | Requires immediate treatment, possible liver transplant | Managed with medications, lifestyle changes, liver transplant in advanced cases |
Various Symptoms of Liver Failure
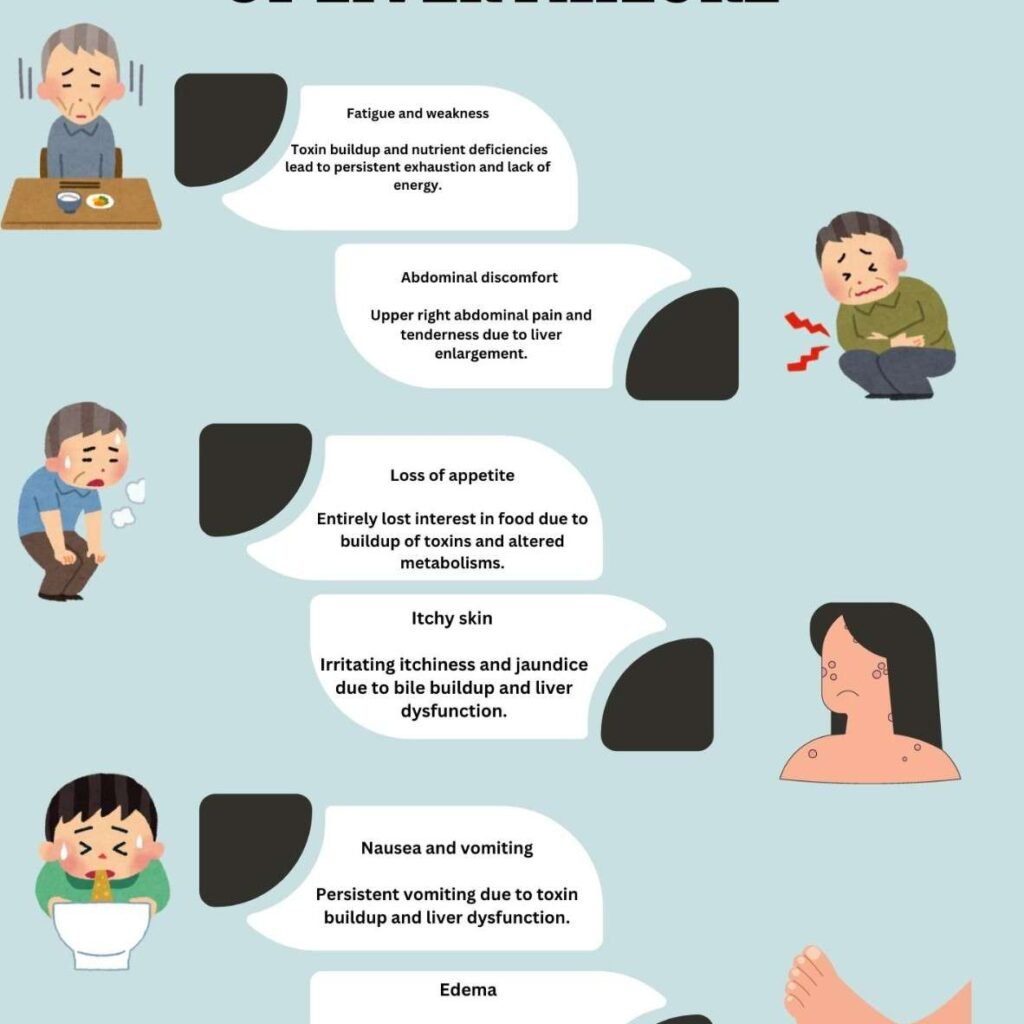
Early Symptoms of Liver Failure
In the initial stages of liver failure, symptoms can be subtle and often mistaken for other health issues. These early signs are important to recognize as they indicate liver stress or damage before significant deterioration occurs.
- Fatigue and Weakness: One of the earliest and most common symptoms of liver failure is an overwhelming sense of fatigue and weakness. This fatigue can be constant, even after adequate rest, and progressively worsens.
- Loss of Appetite: People in the early stages of liver failure often experience a significant loss of appetite. The liver is essential in regulating digestion and metabolism. As liver function deteriorates, it can lead to an aversion to food, sometimes coupled with unexplained weight loss.
- Nausea and Vomiting: As the liver struggles to process and eliminate toxins, nausea and vomiting may occur. The buildup of waste products in the blood due to impaired detoxification can irritate the gastrointestinal system, leading to persistent nausea.
- Abdominal Discomfort: A dull ache or discomfort in the upper right quadrant of the abdomen, where the liver is located, is another early symptom. This sensation is often caused by the liver becoming inflamed or enlarged due to damage.
Progressive Symptoms of Liver Failure
As liver failure progresses, more severe and distinct symptoms begin to emerge. At this stage, liver function is significantly impaired, and the body exhibits clearer signs of distress.
- Jaundice: Jaundice is a classic symptom of liver failure and is characterized by a yellowing of the skin and eyes. It occurs due to the liver’s inability to properly process bilirubin, a yellow pigment formed by the breakdown of red blood cells. As bilirubin accumulates in the bloodstream, it leads to the yellow discoloration of tissues.
- Dark Urine and Pale Stools: Liver failure can cause changes in urine and stool color. Urine becomes dark due to the excess bilirubin being excreted by the kidneys, while stools may become pale or clay-colored due to reduced bile production by the liver. Bile is responsible for the brown color of stool, and when bile flow is disrupted, stool color changes accordingly.
- Swelling (Edema): Fluid retention, particularly in the legs, ankles, and abdomen (a condition known as ascites), is a symptom of worsening liver function. The liver produces albumin, a protein that helps regulate blood volume and pressure. When the liver fails, albumin levels drop, causing fluid to leak from blood vessels into surrounding tissues.
- Itchy Skin (Pruritus): Persistent itching is a common complaint in liver failure and is often associated with the buildup of bile salts under the skin. The exact mechanism is not fully understood, but it is believed that the accumulation of these substances triggers nerve endings in the skin, causing itching that can be severe and distressing.
Advanced Symptoms of Liver Failure
In the advanced stages of liver failure, the body undergoes systemic failure, and symptoms become life-threatening. Immediate medical intervention is necessary at this point.
- Hepatic Encephalopathy: As liver function declines, toxins such as ammonia build up in the bloodstream and can cross the blood-brain barrier, leading to hepatic encephalopathy. Symptoms include confusion, disorientation, difficulty concentrating, personality changes, and, in severe cases, coma. This is a critical and life-threatening condition.
- Bruising and Bleeding: The liver produces clotting factors, proteins that are essential for blood clotting. In liver failure, the production of these proteins is impaired, leading to easy bruising, frequent nosebleeds, or excessive bleeding from minor injuries. In advanced cases, internal bleeding can occur, which may be fatal.
- Enlarged Spleen (Splenomegaly): Liver failure can lead to portal hypertension, a condition where increased pressure in the portal vein (which carries blood from the intestines to the liver) causes blood to back up and enlarge the spleen. An enlarged spleen can contribute to anemia, thrombocytopenia (low platelet count), and increased susceptibility to infections.
- Muscle Wasting: Severe liver failure can lead to muscle wasting and malnutrition, as the liver is central to protein synthesis and nutrient metabolism. The body starts to break down muscle tissue to meet energy demands, leading to muscle weakness and significant weight loss.
Severe Ascites and Fluid Retention: Ascites, the buildup of fluid in the abdomen, worsens in advanced liver failure. This causes the abdomen to swell, sometimes to an extreme degree, and is often accompanied by shortness of breath due to pressure on the diaphragm.
Acute Liver Failure Symptoms
Acute liver failure, also known as fulminant liver failure, is a rapid onset condition that can develop within days or weeks in individuals with no previous liver disease. Symptoms may include:
- Sudden Jaundice
- Severe Mental Confusion (Hepatic Encephalopathy)
- Severe Nausea and Vomiting
- Bleeding Easily
- Multi-organ Failure (as the condition progresses)
Natural Remedies for Liver Failure
Important to note that natural remedies should complement traditional treatments and should always be used under the guidance of a healthcare provider, especially in cases of advanced liver disease or failure.
Milk Thistle (Silybum marianum)
- Active Component: Silymarin, a group of compounds found in milk thistle, is known for its antioxidant, anti-inflammatory, and liver-protective properties. Silymarin works by stabilizing liver cell membranes and promoting the regeneration of damaged liver cells.
- Scientific Evidence: Clinical studies have shown that milk thistle can improve liver function tests in people with liver damage due to conditions such as alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), and hepatitis C. Its antioxidant properties help neutralize free radicals, which cause liver inflammation and damage.
- Use: Milk thistle is typically taken as a supplement in capsule or liquid form. Recommended doses vary, but typical dosages range from 140-420 mg of silymarin per day.
Dandelion Root (Taraxacum officinale)
- Traditional Use: Dandelion root has been used in traditional medicine to treat liver and gallbladder issues for centuries. It is believed to stimulate bile production, helping the liver in detoxifying the body.
- Liver Detoxification: Dandelion root contains antioxidants such as beta-carotene that may help protect the liver from oxidative stress. Additionally, it may support liver function by increasing bile flow, which aids in the digestion of fats and the removal of toxins.
- Use: Dandelion root is available as a tea, tincture, or supplement. Drinking dandelion root tea regularly may help support liver health, but caution should be used in people with bile duct or gallbladder issues, as it can increase bile production.
Turmeric (Curcuma longa)
- Active Compound: Curcumin, the active component in turmeric, is known for its potent anti-inflammatory and antioxidant properties. These qualities may help reduce liver inflammation and oxidative stress, both of which contribute to liver damage.
- Research Findings: Studies suggest that curcumin can help reduce liver inflammation and fibrosis, making it beneficial for conditions like NAFLD and liver cirrhosis. It has also been shown to lower liver enzyme levels in people with liver damage, indicating improved liver function.
- Use: Turmeric can be consumed in food, taken as a supplement, or consumed as tea. For therapeutic effects, standardized curcumin supplements (with 95% curcuminoids) are often recommended, with doses ranging from 500-2,000 mg per day. Adding black pepper to turmeric can improve the absorption of curcumin.
Licorice Root (Glycyrrhiza glabra)
- Active Component: Glycyrrhizin is the primary compound in licorice root that has liver-protective effects. It has anti-inflammatory and antiviral properties and is traditionally used in Chinese medicine to treat liver diseases.
- Liver Health Benefits: Studies have found that glycyrrhizin can help reduce liver inflammation, particularly in patients with chronic hepatitis. It may also help protect against liver damage caused by toxins or viruses.
- Use: Licorice root can be taken in the form of tea, capsules, or liquid extracts. However, long-term use of licorice root may lead to side effects like high blood pressure or low potassium levels, so it should be used under medical supervision.
- Artichoke (Cynara scolymus)
- Liver Regeneration: Artichoke extract is believed to stimulate the regeneration of liver cells and improve liver function. It has been used in traditional medicine to support bile production and promote liver detoxification.
- Research: Some studies have shown that artichoke extract can help lower liver enzyme levels in people with liver disease and may improve symptoms associated with liver dysfunction, such as bloating, nausea, and digestive issues.
- Use: Artichoke leaf extract is typically available as a supplement. Dosages vary, but 600-1,800 mg per day is common in research studies.
Dietary Approaches to Support Liver Health
The liver is heavily involved in the digestion and processing of food, and certain dietary changes can help alleviate stress on the liver and promote healing.
1.Antioxidant-Rich Foods
- Fruits and Vegetables: A diet high in fruits and vegetables provides essential vitamins, minerals, and antioxidants that help reduce oxidative stress on the liver. Some of the best foods for liver health include:
- Cruciferous vegetables (broccoli, Brussels sprouts, cauliflower) that contain compounds like sulforaphane, which support detoxification and may help prevent liver damage.
- Leafy greens (spinach, kale, Swiss chard) that are high in antioxidants like vitamin C and E, which help neutralize free radicals.
- Berries (blueberries, strawberries) rich in polyphenols, which have been shown to reduce liver inflammation and fibrosis.
2.Healthy Fats
- Omega-3 Fatty Acids: Found in fatty fish like salmon, sardines, and flaxseeds, omega-3 fatty acids help reduce liver fat and inflammation, making them particularly beneficial for people with NAFLD or other liver diseases.
- Avoiding Trans Fats and Saturated Fats: Processed foods and fried foods high in trans fats and saturated fats can contribute to fatty liver disease and worsen liver inflammation.
3. Fiber-Rich Foods
- Whole Grains: Foods rich in fiber, such as whole grains (quinoa, oats, brown rice) and legumes, can help regulate blood sugar levels, reduce fat accumulation in the liver, and improve liver function. Fiber also promotes a healthy gut microbiome, which plays a role in liver health.
4.Herbal Teas
- Green Tea: Green tea is rich in catechins, a type of antioxidant that has been shown to improve liver function and reduce fat buildup in the liver. Drinking 2-3 cups of green tea daily may have beneficial effects on liver health, but high-dose green tea supplements should be used cautiously as they may cause liver toxicity.
- Ginger Tea: Ginger has anti-inflammatory and antioxidant properties that can help reduce inflammation in the liver and improve digestion. Drinking ginger tea can promote liver detoxification and alleviate symptoms like bloating and nausea in individuals with liver disease.
Treatment for Liver Failure
In the United States, liver failure treatment follows a multidisciplinary approach that incorporates both advanced medical therapies and supportive care. The treatment methods for liver failure vary depending on the cause, severity, and progression of the disease, and they often involve addressing the underlying condition while managing the complications associated with liver dysfunction
Hospitalization and Intensive Care
The treatment for ALF in the USA focuses on immediate hospitalization and intensive care management, as the condition can lead to multi-organ failure if not promptly addressed.Supportive care is critical to maintaining stability. Medical teams often focus on:
- Hemodynamic Support: Stabilizing blood pressure and maintaining fluid balance with intravenous fluids or vasopressors.
- Respiratory Support: Patients with severe ALF may require mechanical ventilation to support breathing, particularly if encephalopathy or coma develops.
- Acetaminophen (Paracetamol) Overdose: In the USA, acetaminophen toxicity is a leading cause of ALF. The primary treatment is N-acetylcysteine (NAC), administered intravenously. NAC acts as an antidote by replenishing glutathione levels in the liver, which helps detoxify acetaminophen and prevent further damage. Studies show that early administration of NAC can significantly improve survival rates.
- Viral Hepatitis: For patients with ALF caused by viral hepatitis (e.g., hepatitis B or A), specific antiviral treatments may be used. In hepatitis B, for example, lamivudine or tenofovir may be prescribed to inhibit viral replication. Supportive care remains essential as the liver may recover with time if viral replication is controlled.
- Toxin-Induced ALF: Exposure to environmental toxins or drugs (such as Amanita mushroom poisoning) may lead to ALF. In these cases, specific antidotes are administered when available. For example, penicillin G or silymarin (milk thistle extract) is sometimes used in mushroom poisoning to protect liver cells.
- Autoimmune Hepatitis: In cases of autoimmune hepatitis leading to ALF, high-dose corticosteroids like prednisone are administered to suppress the immune system and reduce liver inflammation. Immunosuppressants like azathioprine may also be used to maintain remission.
Liver transplantation
- Eligibility and Evaluation: In the USA, patients with cirrhosis and end-stage liver disease are evaluated for liver transplantation using the MELD score, which takes into account blood tests such as bilirubin, creatinine, and INR (a measure of blood clotting). The higher the MELD score, the more urgent the need for a transplant.
- Transplant Success Rates: Liver transplantation offers a high success rate, with post-transplant survival rates exceeding 80% at one year and 70% at five years. The most common causes of liver transplantation in the USA are alcoholic liver disease, hepatitis C, and NAFLD.
Liver function tests (LFTs)
Liver function tests (LFTs) are a group of blood tests that help assess the health of the liver by measuring the levels of proteins, liver enzymes, and bilirubin in the blood. These tests help diagnose liver disease, monitor the progression of liver conditions, and assess the effects of medications that may impact the liver.
- Alanine Aminotransferase (ALT): Measures the amount of ALT enzyme, which is released into the bloodstream when the liver is damaged.
- Aspartate Aminotransferase (AST): Similar to ALT, this enzyme is found in liver cells and is released into the blood when the liver or muscles are damaged.
- Alkaline Phosphatase (ALP): An enzyme found in the liver and bones, ALP levels can indicate liver disease or bone disorders.
- Bilirubin: A substance produced from the breakdown of red blood cells, bilirubin levels indicate how well the liver is processing waste.
- Albumin: A protein made by the liver, albumin levels help evaluate liver’s synthetic function and overall health.
- Gamma-Glutamyl Transferase (GGT): An enzyme that helps detect bile duct problems, liver disease, or alcohol use.
- Total Protein: Measures the total amount of protein in the blood, including albumin and other proteins, to assess liver function.
- Prothrombin Time (PT): Measures how long it takes for blood to clot. Prolonged PT can suggest liver dysfunction.
| Test | Normal Range | What it indicates |
| Alanine Aminotransferase (ALT) | 7 to 56 U/L | Elevated in liver damage, especially from hepatitis. |
| Aspartate Aminotransferase (AST) | 10 to 40 U/L | Elevated in liver damage, but also in heart or muscle injury. |
| Alkaline Phosphatase (ALP) | 44 to 147 U/L | High levels may indicate liver or bone disorders. |
| Bilirubin (Total) | 0.1 to 1.2 mg/dL | High levels may indicate liver dysfunction or bile duct issues. |
| Albumin | 3.5 to 5.0 g/dL | Low levels suggest liver disease or malnutrition. |
| Gamma-Glutamyl Transferase (GGT) | 9 to 48 U/L | Elevated levels may indicate bile duct problems or alcohol use. |
| Total Protein | 6.3 to 7.9 g/dL | Low levels may indicate liver disease or kidney problems. |
| Prothrombin Time (PT) | 11 to 13.5 seconds | Prolonged time suggests liver dysfunction affecting clotting. |
Liver Biopsy
A liver biopsy is a medical procedure that involves removing a small sample of liver tissue. This sample helps diagnose liver diseases and assess liver function.
A liver biopsy serves as a crucial tool in diagnosing various liver conditions, including hepatitis, cirrhosis, and fatty liver disease. By analyzing the tissue sample, healthcare providers can determine the extent of damage and guide treatment options. The procedure can be performed using different techniques, such as percutaneous, transjugular, or laparoscopic methods.
Patients often undergo this biopsy if blood tests or imaging scans indicate potential liver issues. Understanding the reasons for a liver biopsy can help alleviate concerns and prepare patients for what to expect during the procedure.
What Is Liver Biopsy
A liver biopsy is a medical test that helps doctors check the health of the liver. This test involves taking a small sample of liver tissue. It helps diagnose liver diseases, infections, and other problems. Knowing what a liver biopsy is and its purpose is important for understanding liver health.
Purpose
The main purpose of a liver biopsy is to diagnose liver conditions. Here are some key reasons why a liver biopsy is performed:
- To find out the cause of liver problems.
- To check for liver diseases like hepatitis.
- To see if there is liver damage or scarring.
- To assess the severity of liver conditions.
- To guide treatment options for liver diseases.
Doctors may recommend a liver biopsy if blood tests show unusual liver function. Imaging tests may also indicate liver issues. By examining the liver tissue, doctors can make a clearer diagnosis. This helps in deciding the best treatment plan. The biopsy can also help monitor diseases over time.
Types
There are different types of liver biopsies. Each type has its own method and purpose. Here are the most common types:
| Type of Biopsy | Description |
|---|---|
| Needle Biopsy | A thin needle removes a small piece of liver tissue. |
| Laparoscopic Biopsy | A small camera helps guide the needle to the liver. |
| Surgical Biopsy | Involves a larger incision to get a bigger sample. |
Each type of biopsy has its own benefits. Needle biopsies are often done in a doctor’s office. They are less invasive. Laparoscopic biopsies are done in a hospital. They allow doctors to see the liver closely. Surgical biopsies are less common but provide larger samples.
Procedure Steps
A liver biopsy is a medical procedure that helps doctors check the health of the liver. It involves taking a small piece of liver tissue for testing. This procedure is important for finding liver diseases or conditions. Understanding the procedure steps can help patients prepare for what to expect.
Preparation
Preparing for a liver biopsy is an important step. Patients should follow specific guidelines to ensure safety and success. Here are some key points to consider:
- Discuss medications: Inform the doctor about all medications being taken.
- Avoid certain foods: Patients may need to fast for a few hours before the procedure.
- Arrange transportation: It is wise to have someone drive you home afterward.
- Wear comfortable clothing: Loose-fitting clothes make the procedure easier.
Doctors may also perform some tests before the biopsy. These tests can include:
| Test Name | Purpose |
|---|---|
| Blood Tests | Check liver function and clotting ability. |
| Imaging Tests | Provide a clear view of the liver. |
Following these preparation steps helps ensure a smooth procedure. Patients should feel ready and informed.
Execution
The execution of a liver biopsy involves specific steps. Understanding these steps can ease any anxiety. Here’s how the procedure typically goes:
- Anesthesia: A local anesthetic numbs the area where the biopsy will happen.
- Positioning: Patients lie down, often on their back or side.
- Needle insertion: A thin needle is inserted into the liver to collect tissue.
- Tissue sample: The doctor collects a small sample of liver tissue.
- Monitoring: After the procedure, patients are monitored for a short time.
Most liver biopsies take only a few minutes. Patients may feel some discomfort but usually do not experience severe pain. The doctor will provide care instructions after the procedure. Understanding these steps can help patients feel more comfortable.
Types Of Liver Biopsy
The liver biopsy is a medical test used to check liver health. It helps doctors see if there are any problems in the liver. There are different types of liver biopsy. Each type has its own way of getting a sample. This article explains two main types: percutaneous and transjugular liver biopsies.
Percutaneous
The percutaneous liver biopsy is the most common type. This method involves a thin needle. The needle goes through the skin to get a small piece of liver tissue. Here are some key points about this procedure:
- Performed under local anesthesia.
- Quick and usually takes less than 30 minutes.
- Patients may feel mild pain or discomfort.
- Doctors use ultrasound or CT scans to guide the needle.
After the biopsy, patients may need to rest for a few hours. Most can go home the same day. It is important to follow doctor’s instructions after the procedure. Here’s a simple table showing the pros and cons:
| Pros | Cons |
|---|---|
| Quick recovery time | Risk of bleeding |
| Minimally invasive | May cause discomfort |
Transjugular
The transjugular liver biopsy is different from the percutaneous method. This procedure involves accessing the liver through a vein in the neck. Doctors use a special tube called a catheter. This method is often used for patients with bleeding risks. Here are some important points:
- Performed under local anesthesia and sedation.
- Takes longer than percutaneous biopsy.
- Doctors can also check blood flow in the liver.
- Less risk of bleeding compared to other methods.
After this biopsy, patients may stay in the hospital for a short time. Recovery is usually smooth, but monitoring is essential. Below is a comparison table for easy reference:
| Pros | Cons |
|---|---|
| Safer for high-risk patients | More complex procedure |
| Can assess blood flow | Longer recovery time |
Risks Involved
Liver biopsies are important medical tests. They help doctors see if the liver is healthy. Like any medical procedure, liver biopsies come with risks. Knowing these risks can help patients make informed choices.
Common Risks
Many people face some common risks during a liver biopsy. These risks are usually mild and can be managed easily. Here are some of the most common risks:
- Bleeding: Some bleeding may occur at the biopsy site.
- Pain: Mild pain or discomfort is common after the procedure.
- Infection: There is a small chance of getting an infection.
Most patients recover quickly from these issues. Doctors monitor patients closely after the biopsy. A table below shows the percentage of patients experiencing these risks:
| Risk | Percentage of Patients |
|---|---|
| Bleeding | 1-3% |
| Pain | 10-20% |
| Infection | 0.5-1% |
Rare Complications
While most risks are mild, some rare complications can happen. These complications are serious but very uncommon. Here are a few rare complications:
- Punctured lung: This can happen if the needle goes too deep.
- Severe bleeding: Some patients may need a blood transfusion.
- Damage to blood vessels: This can lead to serious issues.
Doctors take steps to avoid these complications. Most patients do not face these serious problems. Patients should feel comfortable asking their doctors about these risks. Understanding the rare complications can ease worries.
Aftercare
Liver biopsy is a test to check the health of your liver. After the procedure, proper care is essential. Following the right aftercare will help in quick recovery. It is important to follow your doctor’s advice for the best results.
Post-procedure Instructions
After a liver biopsy, certain instructions are crucial to follow. These guidelines ensure a smooth recovery and minimize risks.
- Rest: Take it easy for at least 24 hours.
- Avoid heavy lifting: Do not lift anything over 10 pounds for a week.
- Watch for symptoms: Look for signs of pain or bleeding.
- Hydration: Drink plenty of fluids, especially water.
- Medication: Take pain relievers as directed by your doctor.
It is also important to keep the biopsy site clean and dry. Here’s a simple table to track your symptoms:
| Date | Symptoms | Notes |
|---|---|---|
| Day 1 | Pain, bleeding, fever | Contact doctor if symptoms worsen. |
| Day 2 | Minor discomfort | Normal recovery. |
Follow-up Visits
Follow-up visits are important after a liver biopsy. These check-ups help your doctor see how well you are healing.
During these visits, your doctor will:
- Review biopsy results: Understand what the results mean for your health.
- Check recovery: Ensure that you are healing properly.
- Discuss further tests: If needed, your doctor may suggest more tests.
Scheduling your follow-up is vital. Usually, a visit occurs within one to two weeks after the procedure. Bring a list of any questions or concerns to discuss.
Interpreting Results
A liver biopsy is a procedure used to collect a small sample of liver tissue. Doctors analyze this tissue to understand liver health. Interpreting the results can help diagnose various liver diseases. Knowing what normal and abnormal findings mean is crucial for treatment.
Normal Findings
Normal findings from a liver biopsy indicate that the liver is healthy. The tissue sample shows no signs of disease. Some key points about normal findings include:
- No inflammation present in the liver tissue.
- No fibrosis or scarring in the liver.
- No signs of fatty liver or steatosis.
- No evidence of tumors or abnormal growths.
Here is a simple table showing normal liver biopsy results:
| Finding | Status |
|---|---|
| Inflammation | Absent |
| Fibrosis | Absent |
| Fatty Change | Absent |
| Lesions | None |
Normal liver biopsy results suggest that the liver functions well. Regular check-ups can help maintain liver health.
Abnormal Findings
Abnormal findings from a liver biopsy indicate possible liver problems. This may include various diseases and conditions. Some important points to note are:
- Inflammation may indicate hepatitis.
- Fibrosis can show chronic liver disease.
- Fatty liver may suggest obesity or alcohol use.
- Tumors can indicate cancer or other growths.
Here is a simple table showing common abnormal findings:
| Finding | Possible Condition |
|---|---|
| Inflammation | Hepatitis |
| Fibrosis | Chronic Liver Disease |
| Fatty Change | Non-Alcoholic Fatty Liver Disease |
| Lesions | Liver Cancer |
Abnormal results need careful follow-up with a doctor. Treatment may be necessary to improve liver health.
Alternatives To Biopsy
Liver biopsy is a medical procedure used to diagnose liver diseases. It involves taking a small tissue sample from the liver. Some people may seek alternatives to a liver biopsy for various reasons. Luckily, there are effective methods to assess liver health without surgery. This post explores two main alternatives: imaging techniques and blood tests.
Imaging Techniques
Imaging techniques can provide valuable information about the liver. These methods help doctors visualize the liver without needing a biopsy. Common imaging techniques include:
- Ultrasound: Uses sound waves to create images of the liver.
- CT Scan: Provides detailed cross-sectional images of the liver.
- MRI: Uses magnets and radio waves for detailed liver images.
Each technique has its benefits:
| Technique | Benefits |
|---|---|
| Ultrasound | Safe, quick, and painless. No radiation is used. |
| CT Scan | High-resolution images. Good for detecting tumors. |
| MRI | Excellent for soft tissue. No radiation exposure. |
These imaging techniques help doctors monitor liver conditions effectively. They can assess liver size, structure, and blood flow. Many patients prefer these methods due to their non-invasive nature.
Blood Tests
Blood tests are another alternative to liver biopsy. They can measure liver enzymes and other substances in the blood. This information helps doctors understand liver health. Some common blood tests include:
- ALT and AST: Measure liver enzyme levels.
- ALP: Assesses bile duct function.
- Bilirubin: Indicates liver’s ability to process waste.
Blood tests can provide quick results and are less invasive. They help identify liver diseases like hepatitis and fatty liver. Regular blood tests can track the progression of liver diseases.
Doctors often combine blood tests with imaging techniques for a complete assessment. These methods are effective for many patients. They offer a safer way to monitor liver health without surgery.
Living With Liver Conditions
A liver biopsy is a medical test used to check liver health. It helps doctors find problems like liver disease or damage. Living with liver conditions can be tough, but understanding diet and lifestyle choices can make a big difference. Keeping track of health is also important for managing liver issues.
Diet And Lifestyle
Eating healthy is very important for people with liver conditions. A balanced diet can help keep the liver working well. Here are some key points to remember:
- Eat plenty of fruits and vegetables. They are full of vitamins and minerals.
- Choose whole grains. Foods like brown rice and whole wheat bread are great.
- Limit fatty foods. Avoid fried foods and too much red meat.
- Stay hydrated. Drink plenty of water throughout the day.
- Reduce sugar intake. Too much sugar can harm the liver.
Here is a simple table showing foods to eat and avoid:
| Foods to Eat | Foods to Avoid |
|---|---|
| Fruits (e.g., apples, bananas) | Processed snacks (e.g., chips, cookies) |
| Vegetables (e.g., spinach, carrots) | High-fat dairy products (e.g., cream, cheese) |
| Lean proteins (e.g., chicken, fish) | Red meat (e.g., beef, pork) |
| Whole grains (e.g., oats, quinoa) | Sugary drinks (e.g., soda, energy drinks) |
Monitoring Health
Regular health check-ups are key for managing liver conditions. Keeping track of symptoms helps doctors provide better care. Here are some important steps:
- Schedule regular doctor visits. Regular check-ups help catch problems early.
- Keep a symptom diary. Write down any changes or new symptoms.
- Follow lab tests. Blood tests help monitor liver function.
- Stay active. Exercise can improve overall health.
- Take medications as prescribed. Do not skip doses or change medications without talking to a doctor.
Using a health tracker app can help manage these tasks. It can remind you of appointments and track symptoms easily.
How do I know if I’m at risk for liver problems?
To determine if you’re at risk for liver problems, assess your lifestyle, family history, and any existing health conditions. Common risk factors include obesity, excessive alcohol consumption, and viral hepatitis.
Liver health is crucial for overall well-being. The liver processes nutrients, detoxifies harmful substances, and supports digestion. Recognizing potential risks is essential for prevention. Factors such as age, diet, and medical history can significantly influence liver health. Individuals with a family history of liver disease or those who engage in high-risk behaviors should be particularly vigilant.
Routine medical check-ups and blood tests can help identify early signs of liver dysfunction. Understanding these risks empowers individuals to make healthier lifestyle choices and seek timely medical advice.
Common Symptoms
Understanding liver health is important. The liver plays a key role in our body. Recognizing common symptoms can help you know if you may be at risk for liver problems. Some signs can be easy to overlook. Staying informed can lead to better health choices.
Fatigue And Weakness
Feeling tired or weak often is a common symptom of liver issues. This fatigue can be different from regular tiredness. It may not go away with rest. Here are some important points to consider:
- Unusual tiredness may affect daily activities.
- Weakness can make simple tasks hard to complete.
- Fatigue may increase over time.
- Rest may not relieve this tiredness.
Sometimes, this fatigue is linked to liver function. The liver helps process nutrients and energy. When it is not working well, energy levels can drop. Here is a simple table that shows how liver health affects energy:
| Liver Health Status | Energy Level |
|---|---|
| Healthy | Normal |
| At Risk | Low |
| Unhealthy | Very Low |
Jaundice Signs
Jaundice is a noticeable sign of liver problems. It causes the skin and eyes to look yellow. This happens due to a build-up of bilirubin. Bilirubin is a substance made by the liver. Here are some key signs to watch for:
- Yellowing of the skin.
- Yellowing of the eyes.
- Dark urine may also occur.
- Pale stools can be a sign too.
Jaundice can mean the liver is not working properly. It is important to see a doctor if you notice these signs. Early detection can lead to better health outcomes. Regular check-ups help catch issues early.
Risk Factors
Understanding your risk for liver problems is very important. Many factors can affect liver health. Recognizing these risk factors can help in preventing serious issues. This guide covers two major risk factors: alcohol consumption and obesity. Knowing these can lead to better health choices.
Alcohol Consumption
Alcohol consumption is a significant risk factor for liver problems. Drinking too much alcohol can harm liver cells. Over time, this damage can lead to serious conditions like cirrhosis or fatty liver disease.
Here are some key points about alcohol and liver health:
- Moderate drinking is usually safe for most adults.
- Heavy drinking can cause liver inflammation.
- Binge drinking is especially harmful.
- Women are more sensitive to alcohol than men.
To understand the risks, check out this table:
| Drinking Level | Risk Level |
|---|---|
| Moderate (1 drink/day for women, 2 for men) | Low |
| Heavy (more than 3 drinks/day for women, 4 for men) | High |
| Binge (5 or more drinks in a short time) | Very High |
Regular check-ups with a doctor can help monitor liver health. Cutting back on alcohol can lower the risk of liver damage.
Obesity And Diet
Obesity is another major risk factor for liver problems. Excess weight can lead to fatty liver disease. This happens when fat builds up in liver cells, causing inflammation.
Diet plays a big role in managing weight. Here are some dietary tips:
- Eat more fruits and vegetables.
- Limit sugary drinks.
- Choose whole grains over refined grains.
- Watch portion sizes.
Check out this table for more insights:
| Food Type | Impact on Liver |
|---|---|
| Fruits & Vegetables | Positive |
| Processed Foods | Negative |
| High Sugar Foods | Negative |
Maintaining a healthy weight is crucial for liver health. Regular exercise also helps in managing weight effectively.
Family History
Understanding your risk for liver problems is important. Family history plays a big role in this. Knowing your family’s health can help you take action early. Some liver issues are passed down through genes. This post will help you learn about genetic conditions and inherited liver diseases.
Genetic Conditions
Genetic conditions can affect liver health. These are disorders that run in families. Here are some common genetic liver conditions:
- Hemochromatosis: Too much iron builds up in the body.
- Wilson’s Disease: Copper accumulates in the liver and brain.
- Alpha-1 Antitrypsin Deficiency: A protein that protects the liver is missing or low.
Testing can help find these conditions early. Doctors may suggest:
| Test | Purpose |
|---|---|
| Blood tests | Check for iron and copper levels. |
| Genetic testing | Look for specific gene mutations. |
| Imaging tests | See the liver’s condition. |
Knowing your family’s health history can help. Talk to your doctor if you have concerns.
Inherited Liver Diseases
Inherited liver diseases are passed down from parents to children. These diseases can lead to serious liver issues. Some well-known inherited liver diseases include:
- Cystic Fibrosis: Can affect liver function and cause blockages.
- Glycogen Storage Diseases: Body can’t store sugar properly.
- Familial Hypercholesterolemia: High cholesterol levels can harm the liver.
Early diagnosis is key. Understanding your family history helps identify risks. Speak with family members about any liver issues. Sharing this information with your doctor can lead to better care.
Medical Conditions
Knowing your risk for liver problems is important. Many people do not realize that certain medical conditions can affect liver health. Conditions like diabetes and high cholesterol can lead to serious issues. Understanding these risks can help you take action.
Diabetes Impact
Diabetes can greatly affect liver health. High blood sugar levels can lead to fat buildup in the liver. This condition is known as non-alcoholic fatty liver disease (NAFLD). Here are some key points to consider:
- People with diabetes are more likely to develop liver issues.
- Insulin resistance can worsen liver fat levels.
- Regular monitoring of blood sugar is essential.
Studies show that about 70% of people with diabetes may have liver problems. A healthy diet and regular exercise can help manage diabetes. This, in turn, can protect your liver. Regular check-ups with your doctor are also important for liver health.
Cholesterol Levels
High cholesterol can lead to liver problems as well. The liver plays a key role in processing fats. Too much cholesterol can cause fat to build up in the liver. Here are some important facts:
- High LDL cholesterol can increase the risk of liver disease.
- Maintaining a healthy weight can lower cholesterol levels.
- Regular exercise helps improve cholesterol levels.
Eating a balanced diet is important for keeping cholesterol in check. Foods rich in fiber, like fruits and vegetables, can help. Regular blood tests can track cholesterol levels. Knowing your cholesterol can guide you to a healthier lifestyle.
Medication Effects
Understanding your risk for liver problems is crucial. Many factors can affect liver health, including the medications you take. Some common drugs may harm the liver. Recognizing these effects can help you stay healthy.
Common Drugs
Several medications are known to impact liver function. It’s important to be aware of them. Here’s a list of common drugs that can cause liver issues:
- Acetaminophen (Tylenol)
- Statins (cholesterol medications)
- Antibiotics (like amoxicillin)
- Antiepileptic drugs (like phenytoin)
- Certain antifungal medications
The risk factors for liver damage depend on various elements:
| Drug | Risk Level | Notes |
|---|---|---|
| Acetaminophen | High | Overdose can cause severe liver damage. |
| Statins | Moderate | May cause liver enzyme increases. |
| Antibiotics | Low | Rarely cause liver problems. |
Always discuss any concerns with your doctor. Regular check-ups can help monitor liver health.
Herbal Supplements
Herbal supplements are popular for health benefits. However, some can harm the liver. It’s essential to know which ones to avoid. Here are a few herbal supplements that may pose risks:
- Kava
- Comfrey
- Chaparral
- Germander
- Skullcap
These supplements can lead to liver damage. Monitoring your body’s response to them is key. Some symptoms of liver issues include:
- Yellowing skin or eyes (jaundice)
- Dark urine
- Fatigue
- Nausea or vomiting
Consult with a healthcare professional before taking any herbal supplements. They can help you avoid potential liver risks.
Lifestyle Choices
Understanding your risk for liver problems is crucial. Lifestyle choices play a big role in your liver health. Making informed decisions can help you avoid serious issues down the road.
Exercise Habits
Regular exercise is vital for maintaining a healthy liver. It helps control weight and reduces fat buildup in the liver. Here are some key points about exercise and liver health:
- 30 minutes a day: Aim for at least 30 minutes of moderate exercise.
- Types of exercise: Aerobic exercises like walking, cycling, and swimming are beneficial.
- Strength training: Include strength training twice a week to boost metabolism.
Here’s a simple table showing the benefits of regular exercise:
| Type of Exercise | Benefit |
|---|---|
| Aerobic | Improves heart health and reduces fat. |
| Strength Training | Builds muscle and increases metabolism. |
| Flexibility | Improves overall mobility and reduces injury risk. |
Smoking Risks
Smoking poses serious risks to liver health. It can lead to liver disease and other health problems. Here are some important facts:
- Toxins from smoke: They can harm liver cells and cause inflammation.
- Increased risk: Smokers have a higher chance of developing liver cancer.
- Overall health: Quitting smoking improves liver function and overall well-being.
Protecting your liver means avoiding smoking and secondhand smoke. This choice can greatly improve your liver health and reduce your risk of disease.
Routine Screenings
Understanding whether you are at risk for liver problems is essential. Routine screenings play a key role in identifying potential issues early. Regular check-ups help catch liver diseases before they become serious. Knowing what tests are available can guide you in maintaining your liver health.
Blood Tests
Blood tests are vital for checking liver health. They measure various substances in your blood. Key tests include:
- Liver Function Tests (LFTs): Check levels of enzymes and proteins.
- Hepatitis Tests: Identify infections like Hepatitis A, B, and C.
- Alpha-fetoprotein (AFP): Screens for liver cancer.
These tests help doctors see how well your liver is working. Abnormal results may signal liver issues. Here is a simple table of common blood tests:
| Test Name | Purpose |
|---|---|
| Liver Function Tests | Check liver enzymes and proteins |
| Hepatitis Panel | Detect liver infections |
| Alpha-fetoprotein | Screen for liver cancer |
Regular blood tests can catch liver problems early. Talk to your doctor about how often you should get tested.
Imaging Techniques
Imaging techniques help visualize the liver. They provide detailed pictures of its structure. Common imaging methods include:
- Ultrasound: Uses sound waves to create images.
- CT Scan: Offers cross-sectional images of the liver.
- MRI: Uses magnets and radio waves for detailed pictures.
These techniques help find liver damage or tumors. Each method has its own benefits:
| Imaging Technique | Benefits |
|---|---|
| Ultrasound | No radiation, quick and easy |
| CT Scan | Detailed images, good for tumors |
| MRI | Very detailed, no radiation |
Ask your doctor which imaging technique is best for you. They can guide you based on your health history.
When To Seek Help
Many people worry about their health. One important part of health is the liver. Understanding liver health helps everyone know when to seek help. Recognizing the signs of liver problems is key. This guide highlights important signs and what to do next.
Emergency Signs
Recognizing emergency signs is crucial for liver health. Some symptoms may indicate serious issues. Pay attention to the following signs:
- Severe abdominal pain in the upper right side
- Yellowing of the skin or eyes (jaundice)
- Confusion or difficulty thinking clearly
- Unusual bleeding or bruising
- Dark urine or pale stools
Seek immediate help if any of these signs occur. Quick action can save lives. Below is a table of symptoms and their meanings:
| Symptom | Possible Meaning |
|---|---|
| Severe abdominal pain | Possible liver inflammation or damage |
| Yellowing skin/eyes | Jaundice; bile flow issues |
| Confusion | Possible liver failure |
| Unusual bleeding | Coagulation problems |
| Dark urine | Bilirubin buildup |
Being aware of these signs can lead to timely treatment. Don’t ignore your body’s signals.
Consulting A Specialist
Seeing a liver specialist is important for proper care. If you notice any signs of liver issues, consider scheduling an appointment. A specialist can provide detailed information and tests. This helps find any problems early. Here’s when to see a specialist:
- Family history of liver disease
- Persistent fatigue without reason
- Frequent nausea or vomiting
- Changes in appetite or weight
During the visit, the specialist may perform tests like:
- Blood tests to check liver enzymes
- Imaging tests like ultrasound or CT scans
- Liver biopsy if needed
Listening to a specialist can guide you toward a healthier future. Taking action early is key. Your liver health matters.
How Can I Keep My Liver Healthy?
To keep your liver healthy, maintain a balanced diet rich in fruits and vegetables. Regular exercise, limited alcohol intake, and avoiding harmful substances are also essential.
The liver plays a crucial role in detoxification, metabolism, and overall health. A healthy liver supports digestion and energy levels, making it vital for daily functioning. Poor liver health can lead to serious conditions, including fatty liver disease and cirrhosis.
Making simple lifestyle changes can significantly enhance liver function. Consuming nutrient-dense foods, staying hydrated, and managing stress contribute to liver well-being. Regular health check-ups can help monitor liver health, ensuring early detection of potential issues. Prioritizing these practices fosters a healthier, more vibrant life. Protecting your liver today can lead to a healthier tomorrow.
Nutrition Matters
Keeping your liver healthy is very important for your overall well-being. A healthy liver helps your body digest food and filter out toxins. Nutrition plays a key role in keeping your liver in great shape. Eating the right foods and staying hydrated can make a big difference.
Balanced Diet
A balanced diet is essential for liver health. This means eating a mix of different foods. Focus on including fruits, vegetables, whole grains, and lean proteins. Here are some key points to remember:
- Eat plenty of fruits and vegetables. Aim for at least five servings a day.
- Choose whole grains. Foods like brown rice and whole wheat bread are best.
- Limit saturated fats. Avoid fried foods and high-fat meats.
- Incorporate healthy fats. Foods like avocados and nuts are great choices.
- Stay away from sugar. High sugar can harm your liver.
Here is a simple table of liver-friendly foods:
| Food Type | Examples |
|---|---|
| Fruits | Apples, Berries, Oranges |
| Vegetables | Spinach, Broccoli, Carrots |
| Whole Grains | Oats, Quinoa, Brown Rice |
| Lean Proteins | Chicken, Fish, Legumes |
Making these changes can help keep your liver healthy and strong.
Hydration Tips
Staying hydrated is also key for liver health. Water helps your liver flush out toxins. Aim to drink at least eight glasses of water each day. Here are some tips to stay hydrated:
- Carry a water bottle. Having water nearby makes it easier to drink.
- Set reminders. Use your phone to remind you to drink water.
- Drink herbal teas. They can be tasty and help with hydration.
- Eat water-rich foods. Fruits like watermelon and cucumber can help.
Keep an eye on your urine color. A pale yellow color usually means you are well-hydrated. Dark yellow might mean you need to drink more water. Remember, a well-hydrated body supports a healthy liver.
Exercise Regularly
Keeping your liver healthy is important for your overall well-being. One of the best ways to support your liver is to exercise regularly. Exercise can help your liver function better and improve your overall health. This guide will help you understand the types of exercise you can do and how to set achievable fitness goals.
Types Of Exercise
There are many fun and effective ways to exercise. Each type has unique benefits for your liver health:
- Aerobic Exercise: Activities like walking, running, or cycling get your heart pumping.
- Strength Training: Lifting weights or doing body-weight exercises builds muscle.
- Flexibility Exercises: Stretching or yoga improves your body’s flexibility and can reduce stress.
- Balance Training: Activities like tai chi help with stability and coordination.
Here’s a simple table showing different types of exercises and their benefits:
| Type of Exercise | Benefits |
|---|---|
| Aerobic | Improves heart health and boosts liver function. |
| Strength | Increases muscle mass and metabolism. |
| Flexibility | Reduces injury risk and improves posture. |
| Balance | Enhances stability and prevents falls. |
Choosing the right mix of these exercises can greatly benefit your liver health.
Setting Goals
Setting clear goals helps you stay motivated. Goals should be specific, measurable, achievable, relevant, and time-bound (SMART).
Start by asking yourself what you want to achieve. Do you want to run a mile? Or maybe lift a certain weight? Write down your goals.
- Specific: Define your target clearly.
- Measurable: Use numbers to track your progress.
- Achievable: Ensure your goals are realistic.
- Relevant: Make sure your goals support your liver health.
- Time-bound: Set a deadline to reach your goals.
For example, instead of saying, “I want to exercise more,” try “I will walk 30 minutes every day for a month.” This makes it easier to track your progress and stay committed.
Remember, small steps lead to big changes. Celebrate your achievements along the way!
Limit Alcohol Intake
Keeping your liver healthy is very important for your overall well-being. One major way to do this is by limiting alcohol intake. The liver plays a big role in breaking down alcohol. Drinking too much can harm this vital organ. Understanding the guidelines and effects of excess alcohol can help you make better choices.
Recommended Guidelines
Following the recommended guidelines for alcohol consumption can protect your liver. Health experts suggest:
- Men should not drink more than 2 drinks per day.
- Women should limit themselves to 1 drink per day.
- Take at least 2 alcohol-free days each week.
It’s important to know what counts as a standard drink. Here’s a simple table to help you:
| Type of Drink | Standard Drink Size |
|---|---|
| Beer | 12 ounces |
| Wine | 5 ounces |
| Spirits | 1.5 ounces |
Understanding these guidelines can help keep your liver safe. Always remember that moderation is key.
Effects Of Excess
Drinking too much alcohol can have serious effects on the liver. It can lead to conditions like:
- Fatty liver disease: This is when fat builds up in liver cells.
- Alcoholic hepatitis: This causes inflammation of the liver.
- Cirrhosis: This is severe scarring of the liver.
These conditions can result in symptoms like:
- Fatigue and weakness
- Yellowing of the skin or eyes
- Swelling in the abdomen
Excessive drinking can also affect other organs. It can lead to heart problems and digestive issues. Taking care of your liver is essential for a healthy life.
Avoid Toxins
Keeping your liver healthy is very important for your body. It helps to filter toxins and supports digestion. Avoiding toxins is a key way to protect your liver. Knowing where toxins come from helps you stay healthy.
Common Sources
Many everyday items can harm your liver. Here are some common sources of toxins:
- Alcohol: Excessive drinking can damage liver cells.
- Processed foods: These often contain unhealthy fats and sugars.
- Medications: Some drugs can be tough on the liver.
- Environmental pollutants: Chemicals in the air and water can be harmful.
Understanding these sources helps you make better choices. Here is a simple table showing common toxins and their sources:
| Toxin | Source |
|---|---|
| Alcohol | Drinks like beer and wine |
| Acetaminophen | Over-the-counter pain relievers |
| Heavy metals | Contaminated water or food |
| Pesticides | Fruits and vegetables treated with chemicals |
Being aware of these toxins is the first step to keeping your liver safe.
Safe Practices
Many safe practices can help protect your liver. Making small changes in your daily routine is important. Here are some safe practices to consider:
- Drink plenty of water: Staying hydrated helps flush out toxins.
- Eat a balanced diet: Include fruits, vegetables, and whole grains.
- Limit alcohol consumption: Keep it to a minimum to reduce liver strain.
- Exercise regularly: Physical activity supports overall health.
These practices are simple but effective. They can greatly improve your liver health. Following these steps will help you live a healthier life.
Maintain Healthy Weight
Keeping your liver healthy is very important for overall wellness. One key way to support liver health is by maintaining a healthy weight. A balanced weight reduces the risk of liver disease and promotes good liver function.
Weight Management Tips
Managing your weight is essential for liver health. Here are some simple tips to help you:
- Eat a balanced diet: Focus on fruits, vegetables, whole grains, and lean proteins.
- Limit sugar and fat: Avoid sugary drinks and fast food.
- Stay active: Aim for at least 30 minutes of exercise most days.
- Drink plenty of water: Hydration is key for a healthy liver.
- Watch portion sizes: Eating smaller portions can help with weight control.
Consider tracking your meals and snacks. Keeping a food diary can help you stay on track. Here’s a simple table to help you set goals:
| Goal | Action |
|---|---|
| Eat 5 servings of fruits and vegetables | Plan meals with colorful veggies and fruits |
| Exercise 150 minutes a week | Join a fun class or walk with friends |
| Drink 8 glasses of water daily | Carry a water bottle everywhere |
Monitoring Progress
Monitoring your weight helps you stay healthy. Tracking your progress allows you to see changes over time. Here are some ways to monitor your weight effectively:
- Weigh yourself weekly: Choose a consistent day and time.
- Use a journal: Write down your weight and feelings.
- Take measurements: Measure your waist and hips each month.
Set realistic goals for your weight. Celebrate small victories. For example, losing even a few pounds can make a big difference.
Try to get support from family and friends. They can help keep you motivated. Remember, a healthy liver contributes to a healthier you!
Regular Health Check-ups
Keeping your liver healthy is very important for your overall well-being. Regular health check-ups help monitor liver health and catch problems early. These check-ups include tests that can show how well your liver is working. By understanding the importance of screenings, you can take better care of your liver.
Importance Of Screenings
Screenings for liver health are essential for everyone, especially those at risk. They help find problems before they become serious. Here are some key reasons why screenings matter:
- Early Detection: Finding liver issues early can save lives.
- Preventive Care: Screenings help avoid serious diseases.
- Monitoring Health: Regular tests show how well your liver is doing.
Many factors can affect liver health. These include diet, alcohol use, and certain medications. Regular screenings can help identify risks based on these factors. Below is a table that summarizes common liver tests:
| Test Name | Purpose |
|---|---|
| Liver Function Test | Checks how well the liver is working. |
| Ultrasound | Looks at the liver’s size and shape. |
| CT Scan | Provides detailed images of the liver. |
| Biopsy | Takes a small tissue sample for testing. |
What To Expect
During a liver health screening, you will go through several steps. First, a healthcare provider will ask about your medical history. They may also ask about your diet and lifestyle choices. Then, some tests will be done to check your liver function.
Here are some common tests you might experience:
- Blood Tests: These check for liver enzymes and other markers.
- Imaging Tests: Ultrasound or CT scans help visualize the liver.
- Physical Exam: The doctor may check for any signs of liver issues.
Make sure to follow any instructions given before the tests. Some tests may require fasting. Understanding what to expect can make the process easier and less stressful.
Manage Medications
Keeping your liver healthy is very important. It helps your body filter toxins and store nutrients. Managing medications is key to liver health. Taking the right medicines safely can prevent liver damage. Knowing how to use both prescription and over-the-counter drugs is essential.
Prescription Safety
Taking prescription medications safely can protect your liver. Always follow your doctor’s instructions. Here are some tips to ensure safety:
- Read Labels: Always read the labels on your medications.
- Dosage Matters: Take the correct amount as prescribed.
- Alcohol Interaction: Avoid alcohol while on medications.
- Report Side Effects: Tell your doctor about any bad reactions.
Some medications can harm the liver. Here is a table of common prescription drugs and their liver effects:
| Medication | Potential Liver Risk |
|---|---|
| Acetaminophen | Can cause liver damage if overdosed |
| Statins | May raise liver enzymes in some people |
| Antibiotics | Can cause liver injury in rare cases |
Stay in touch with your doctor about any changes in your health. Regular check-ups can help monitor liver health.
Over-the-counter Caution
Over-the-counter (OTC) medications can also affect your liver. Many people think they are safe, but caution is necessary. Read the labels carefully. Here are some important points:
- Know Ingredients: Check for acetaminophen in many products.
- Follow Dosage: Never exceed the recommended dose.
- Mixing Medications: Avoid mixing different OTC drugs.
- Consult a Doctor: Ask a doctor if unsure about a product.
Here are common OTC drugs that may pose a risk to liver health:
| OTC Drug | Liver Risk |
|---|---|
| Acetaminophen | High doses can cause serious damage |
| NSAIDs (like ibuprofen) | Long-term use can harm the liver |
| Cold and flu remedies | Often contain acetaminophen |
Always be aware of what you are taking. Your liver will thank you for it!
Stress Management
Keeping your liver healthy is very important for your overall well-being. The liver helps digest food and remove toxins. Stress can hurt your liver health. Learning to manage stress is key to keeping your liver strong. Using the right techniques can make a big difference.
Relaxation Techniques
Relaxation is a great way to reduce stress. It helps your body and mind feel better. Here are some effective relaxation techniques:
- Deep Breathing: Take slow, deep breaths. Inhale through your nose and exhale through your mouth.
- Progressive Muscle Relaxation: Tense and then relax each muscle group. Start from your toes and work up to your head.
- Yoga: This practice combines movement and breathing. It can help calm your mind.
- Visualization: Picture a peaceful scene. Imagine yourself in a calm place.
Using these techniques regularly can lower stress levels. Create a routine that includes these practices. You can also try this simple table to track your relaxation practices:
| Technique | Frequency |
|---|---|
| Deep Breathing | 3 times a day |
| Yoga | 2 times a week |
| Visualization | Daily |
Mindfulness Practices
Mindfulness helps you stay present. It teaches you to focus on the moment. This can reduce stress and improve liver health.
Here are some simple mindfulness practices:
- Mindful Eating: Pay attention to your food. Chew slowly and enjoy each bite.
- Gratitude Journaling: Write down things you are thankful for. This can improve your mood.
- Nature Walks: Spend time outdoors. Focus on the sights and sounds around you.
- Body Scan Meditation: Notice how each part of your body feels. This can help you relax.
By practicing mindfulness, you can lower stress. Try to include these activities in your daily life. They can make you feel better and improve liver health.
Conclusion
Maintaining a healthy liver is vital for overall well-being. Regular check-ups, a balanced diet, and staying active can make a difference. Avoid excessive alcohol and harmful substances. Simple lifestyle changes can support liver health significantly. Prioritize your liver care, and enjoy a healthier, happier life.
Your body will thank you!


