Pancreatic cancer is one of the most aggressive forms of cancer, and understanding its end stage is crucial for patients, families, and caregivers. This guide provides an in-depth look at end-stage pancreatic cancer, covering diagnosis, symptoms, management, and care, while also addressing the emotional and psychological aspects associated with this phase.
End stage pancreatic cancer
1. Overview of Pancreatic Cancer
Pancreatic cancer arises when cells in the pancreas, a vital part of the digestive system and a gland involved in hormone production, begin to multiply uncontrollably. It often goes undetected until it’s advanced and difficult to treat.
Key Points:
- Incidence and Mortality: It is the fourth leading cause of cancer death in both men and women.
- Risk Factors: Smoking, chronic pancreatitis, diabetes, family history, and certain genetic disorders.
- Types: The most common type is pancreatic adenocarcinoma, accounting for about 90% of cases.
2. Progression to End Stage
The progression of pancreatic cancer can be divided into stages, with end-stage cancer, often referred to as stage IV, indicating that the cancer has spread extensively beyond the pancreas.
Characteristics of End-Stage Pancreatic Cancer:
- Metastasis: Cancer has spread to distant organs, such as the liver, lungs, or peritoneal cavity.
- Symptoms: Severe pain, weight loss, jaundice, and digestive difficulties.
- Treatment Focus: Shifts from curative to palliative, aiming to relieve symptoms and improve quality of life.
3. Diagnosis of End-Stage Pancreatic Cancer
Diagnosing end-stage pancreatic cancer involves several tests to determine the extent of the spread and to assess the patient’s overall condition.
Diagnostic Tools Include:
- Imaging Tests: CT scans, MRI, PET scans, and ultrasounds to visualize the spread.
- Biopsy: A tissue sample taken to confirm the type of pancreatic cancer.
- Blood Tests: Check liver function, kidney function, and markers that may indicate cancer like CA19-9.
4. Symptoms and Management
Symptoms in the end stage can be severe and require comprehensive management strategies.
Common Symptoms and Their Management:
- Pain: Managed with opioids, nerve blocks, or pain pumps.
- Jaundice: Treated with stent placement or biliary drainage if the bile duct is obstructed.
- Digestive Issues: Enzyme supplements and dietary changes help manage malnutrition and weight loss.
- Ascites: Fluid accumulation in the abdomen may be managed with diuretics or paracentesis.
5. Treatment Options at End Stage
While the focus is on palliative care, certain treatments may be applied to manage symptoms and complications.
Treatment Approaches Include:
- Chemotherapy: May be used to slow the spread and manage symptoms.
- Radiation Therapy: Occasionally used to relieve pain or to reduce tumor size for symptom control.
- Clinical Trials: Patients may opt for clinical trials that focus on end-stage cancer treatment.
6. Palliative Care
Palliative care is crucial at this stage and focuses on enhancing quality of life.
Components of Palliative Care:
- Symptom Management: Comprehensive approach to managing pain, nausea, and other symptoms.
- Psychological Support: Counseling for patients and families.
- End-of-Life Planning: Assistance with healthcare directives and planning.
7. Nutritional Support
Nutrition is a significant concern for end-stage pancreatic cancer patients due to appetite loss and malabsorption.
Nutritional Strategies:
- High-calorie, Nutrient-dense Foods: Helps combat weight loss.
- Supplements: Pancreatic enzymes and vitamins may be prescribed.
- Feeding Tubes: In severe cases, tubes may be necessary.
8. Coping with Psychological Impact
The psychological impact on patients and their families can be profound.
Support Mechanisms:
- Counseling: Support groups, therapy, and counseling can help.
- Spiritual Care: Many find comfort in spiritual or religious support.
- Family and Caregiver Support: Education and resources for caregivers.
9. Legal and Ethical Considerations
Patients often need to make decisions about their care preferences and legal matters.
Important Considerations:
- Advance Directives: Patients should be encouraged to make decisions about their care preferences early.
- Power of Attorney: Assigning someone to make decisions when the patient is unable.
- Ethical Considerations: Issues such as the desire for hastened death and withdrawal of support systems.
10. End-of-Life Care
As pancreatic cancer reaches its final stages, end-of-life care becomes the primary focus.
End-of-Life Care Strategies:
- Hospice Care: Provides comprehensive symptom management at home or in a hospice facility.
- Comfort Measures: Focuses on keeping the patient comfortable with medications, therapies, and personal care.
- Family Involvement: Family members are closely involved in care and decision-making.
11. Research and Future Directions
Research continues to explore better ways to treat and manage pancreatic cancer at all stages.
Current Research Focuses:
- New Treatment Modalities: Exploring targeted therapies and immunotherapies.
- Early Detection Methods: Developing better screening tests to catch the disease earlier.
- Quality of Life Studies: Studies that focus on improving the quality of life for end-stage patients.
12. Conclusion
End-stage pancreatic cancer is a challenging phase for patients and their families, requiring a multidisciplinary approach to care that includes medical, psychological, and supportive treatments aimed at maintaining quality of life. As research progresses, there is hope for more effective treatments and better management strategies.

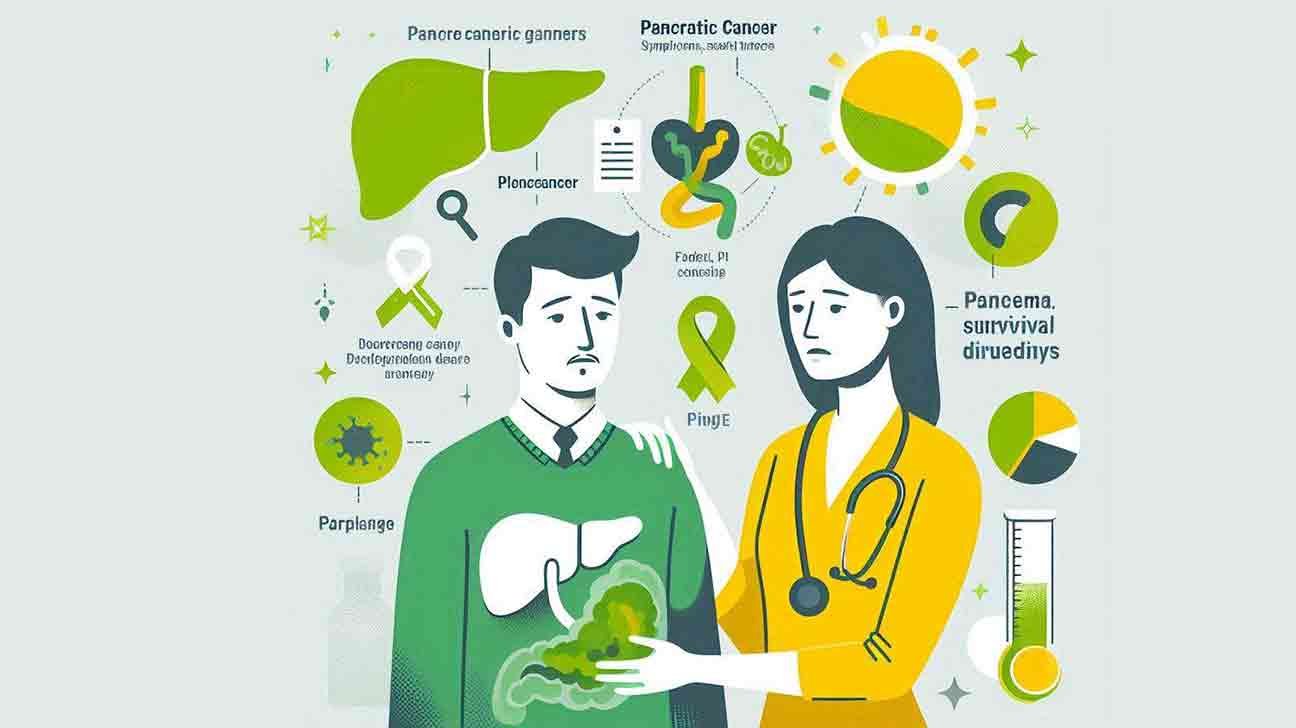
Pancreatic cancer is a type of cancer that affects the pancreas. It is known for its aggressive nature and poor prognosis.
Pancreatic cancer often goes undetected in its early stages, leading to a high mortality rate. Symptoms may include abdominal pain, weight loss, and jaundice. The disease can spread to other organs, making it challenging to treat. Treatment options may include surgery, chemotherapy, and radiation therapy.
Early detection and intervention are crucial in improving outcomes for individuals with pancreatic cancer. Research continues to focus on developing more effective treatments for this deadly disease.
Pancreatic Cancer
Pancreatic cancer is a type of cancer that starts in the pancreas, a small organ behind the stomach. It can be challenging to detect in its early stages and often has a poor prognosis. Common symptoms include abdominal pain, weight loss, and jaundice.
Treatment options may include surgery, chemotherapy, and radiation therapy.
Understanding Pancreatic Cancer
Pancreatic cancer is a type of cancer that develops in the pancreas, an organ located behind the stomach. This aggressive form of cancer is often challenging to detect in its early stages, making treatment difficult. It is essential to understand the symptoms, causes, and available treatments for this disease to improve the chances of early diagnosis and effective management.
Symptoms Of Pancreatic Cancer
- Jaundice: Yellowing of the skin and eyes due to the buildup of bilirubin in the body.
- Abdominal pain: Dull or gnawing pain in the upper abdomen that may spread to the back.
- Unexplained weight loss: Sudden and unexplained loss of weight without changes in diet or physical activity.
Diagnosis And Treatment
Pancreatic cancer diagnosis often involves various imaging tests such as ultrasound, CT scans, MRI scans, and positron emission tomography (PET) scans. These tests help in identifying the presence and extent of the cancer. Treatment options may include surgery, chemotherapy, radiation therapy, or a combination of these approaches, depending on the stage and severity of the cancer.
Causes Of Pancreatic Cancer
- Age: The risk of developing increases with age, with the majority of cases occurring in individuals over 60 years old.
- Smoking: Cigarette smoking is a significant risk factor for pancreatic cancer.
- Family history: Having a family member with pancreatic cancer increases an individual’s risk of developing the disease.
Living With Pancreatic Cancer
Living with pancreatic cancer can be challenging both physically and emotionally. It is crucial for patients to seek support from healthcare professionals, caregivers, and support groups to manage the symptoms and maintain a good quality of life during the treatment process.
Seeking Support And Resources
Patients and their families can benefit from accessing resources and support networks provided by organizations dedicated to pancreatic cancer awareness and research. These resources offer valuable information, guidance, and emotional support to help individuals navigate their journey with pancreatic cancer.
By understanding the symptoms, causes, and available treatments for pancreatic cancer, individuals can take proactive steps towards early detection and effective management of this disease. Seeking support and staying informed about the latest developments in pancreatic cancer research can make a significant difference in the lives of those affected by this condition.
Pancreatic Cancer Symptoms
Pancreatic cancer symptoms may include dull or gnawing pain in the upper abdomen, which may spread to the back, leading to weight loss and abdominal pain as it progresses to advanced stages. Imaging tests and medical consultation are crucial for early diagnosis and treatment.
Recognizing Pancreatic Cancer Symptoms:
- Abdominal Pain: One of the most common symptoms is a dull or gnawing pain in the upper abdomen.
- Back Pain: Pain from pancreatic cancer can spread to the back.
- Pain Variability: Initially, the pain may be intermittent but can become constant as the tumor progresses.
- Pain Triggers: Pain may worsen when lying down or after eating.
- Other Symptoms: Pancreatic cancer may also present with weight loss, jaundice, nausea, and changes in stool color.
Understanding The Significance Of Symptoms:
Pancreatic cancer symptoms are often nonspecific and may mimic other conditions. It is crucial to pay attention to persistent symptoms and seek medical evaluation promptly. If you experience any of these symptoms, especially in combination, consult a healthcare provider for proper assessment and diagnosis.
Early detection can significantly impact treatment outcomes and prognosis.
Seeking Medical Evaluation For Symptoms:
If you notice persistent abdominal or back pain, unexplained weight loss, jaundice, or changes in digestive patterns, it is essential to schedule an appointment with a healthcare professional. Your doctor may recommend further diagnostic tests, such as imaging studies or blood work, to assess your symptoms and determine the underlying cause.
Prompt evaluation and diagnosis are key in managing pancreatic cancer effectively.
Symptoms Of Pancreatic Cancer
Pancreatic cancer symptoms may include dull or gnawing abdominal pain that can spread to the back. Pain intensity varies among individuals, with some experiencing no pain. Advanced stages may manifest with weight loss and persistent abdominal pain.
Pancreatic cancer often goes undetected in its early stages due to a lack of noticeable symptoms. However, as the disease progresses, several symptoms may become apparent. These symptoms can vary from person to person and may include:
- Abdominal Pain: Patients may experience a dull or gnawing pain in the upper abdomen, which may spread to the sides or back. This pain may initially be intermittent but can become more constant and severe as the tumor grows.
- Jaundice: A yellowing of the skin and the whites of the eyes is a common symptom of pancreatic cancer. This occurs when the tumor obstructs the bile duct, causing a build-up of bilirubin in the body.
- Unexplained Weight Loss: Patients may experience unexplained weight loss despite maintaining their regular diet. This can be a result of the cancer affecting the body’s ability to digest and absorb nutrients.
- Loss of Appetite: A reduced appetite and changes in taste preferences are common . Patients may feel full after eating small amounts of food.
- Changes in Stool: Pancreatic cancer can cause changes in stool, including pale, greasy, and foul-smelling stools due to a lack of pancreatic enzymes reaching the intestines.
- Diabetes: New-onset diabetes or unexplained worsening of existing diabetes can be associated with pancreatic cancer. The tumor can affect the pancreas’ ability to produce insulin, leading to high blood sugar levels.
- Nausea and Vomiting: These symptoms may occur as a result of the tumor pressing against the stomach or other organs.
- Fatigue: Patients with pancreatic cancer often experience extreme tiredness and lack of energy, even after adequate rest.
- Blood Clots: The occurrence of blood clots, especially in the veins of the legs, may be a sign of pancreatic cancer.
- Digestive Issues: Pancreatic cancer can lead to digestive problems, such as indigestion, bloating, and discomfort after eating.
Recognizing and understanding these symptoms can aid in the early detection and treatment of pancreatic cancer, potentially improving the prognosis for individuals affected by this disease. If you or someone you know experiences any of these symptoms, it is essential to seek medical attention for proper evaluation and diagnosis.
Pancreatic Cancer Survival Rate
Pancreatic cancer has a low survival rate, with only about 10% of patients living beyond five years after diagnosis. This is due to the aggressive nature of the disease and the lack of early detection methods. Early diagnosis and prompt treatment can significantly improve the chances of survival for pancreatic cancer patients.
Pancreatic cancer is one of the most aggressive and deadliest forms of cancer. Understanding the survival rates associated with this disease is crucial for patients and their families. Here’s a closer look at the and what it means for those affected:
- Survival Rate Statistics:
- The overall 5-year survival rate for pancreatic cancer is dismally low, at around 10%.
- It’s important to note that survival rates can vary depending on several factors, including the stage at which the cancer is diagnosed and the patient’s overall health.
Factors Affecting Survival
Several factors can impact an individual’s chances of surviving pancreatic cancer. These factors include:
- Stage of Cancer:
- Patients diagnosed at an early stage have a higher chance of survival compared to those diagnosed at a later stage when the cancer has spread.
- Treatment Options:
- The type of treatment received, such as surgery, chemotherapy, or radiation therapy, can significantly influence survival rates.
- Overall Health:
- Patients with better overall health and fewer underlying health conditions may have a higher chance of surviving pancreatic cancer.
Improving Survival Rates
While the survival rates for pancreatic cancer may seem discouraging, there are ongoing efforts to improve outcomes for patients. Some potential strategies for enhancing survival rates include:
- Early Detection Initiatives:
- Increasing awareness about the symptoms of pancreatic cancer and promoting regular screenings can lead to earlier detection and improved survival rates.
- Advancements in Treatment:
- Research and development of new treatment options, including targeted therapies and immunotherapies, hold promise for improving survival rates.
- Supportive Care:
- Providing comprehensive supportive care for patients, including pain management and nutritional support, can contribute to better overall outcomes.
Understanding the pancreatic cancer survival rate is essential for patients, caregivers, and healthcare professionals. By addressing the factors that impact survival and advocating for advancements in early detection and treatment, there is hope for improving outcomes in the fight against pancreatic cancer.
Signs Of Pancreatic Cancer
Pancreatic cancer signs may include dull abdominal pain spreading to the back, weight loss, and advanced symptoms like liver metastasis. Early detection through imaging tests is crucial for timely treatment.
Pancreatic cancer is often referred to as a “silent killer” due to the difficulty in early detection. The signs and symptoms may not be noticeable in the initial stages, making it crucial to be aware of the warning signs. Recognizing the can lead to early diagnosis and a higher chance of successful treatment.
Symptoms To Look Out For
- Jaundice: Yellowing of the skin and whites of the eyes due to the buildup of bilirubin.
- Abdominal pain: Dull or gnawing pain in the upper abdomen that may spread to the back.
- Unexplained weight loss: Significant weight loss without any known cause.
- Loss of appetite: A decreased desire to eat, leading to unintended weight loss.
- Changes in bowel movements: Such as diarrhea, constipation, or pale, foul-smelling stools.
Signs That Require Immediate Attention
- New-onset diabetes: The sudden development of diabetes, especially in older individuals with a healthy weight.
- Digestive issues: Including indigestion, nausea, vomiting, or difficulty in digesting fatty foods.
- Blood clots: Development of a blood clot, particularly in the deep veins of the legs.
Recognizing these signs and symptoms is vital for early detection and effective treatment of pancreatic cancer. If you experience any of these warning signs, it is important to consult a healthcare professional promptly for further evaluation.
Stage 4 Pancreatic Cancer
Stage 4 pancreatic cancer is the most advanced stage of pancreatic cancer. At this stage, the cancer has spread to other parts of the body, such as the liver, lungs, or bones, making it difficult to treat. Symptoms include weight loss and abdominal pain.
Early detection is crucial for effective treatment.
Understanding Stage 4 Pancreatic Cancer
Stage 4 pancreatic cancer, also known as metastatic pancreatic cancer, is the most advanced stage of the disease. At this stage, the cancer has spread to other organs in the body, making it challenging to treat. Here’s what you need to know about :
- Metastasis: At this stage, the cancer has spread from the pancreas to other organs, such as the liver, lungs, or abdominal cavity. This makes treatment more complex and may limit the options available for managing the disease.
- Symptoms: Patients with stage 4 pancreatic cancer may experience more severe symptoms, including jaundice, significant weight loss, severe abdominal pain, and digestive issues. These symptoms can significantly impact the patient’s quality of life.
- Prognosis: The prognosis for stage 4 pancreatic cancer is generally poor, with a lower survival rate compared to earlier stages. However, advancements in treatment options and supportive care have improved outcomes for some patients.
- Treatment Options: While curative treatment may not be feasible at this stage, palliative care focuses on managing symptoms and improving the patient’s quality of life. Chemotherapy, radiation therapy, and targeted therapy are often used to slow the progression of the disease and alleviate symptoms.
Coping With Stage 4 Pancreatic Cancer
Coping with a diagnosis of stage 4 pancreatic cancer can be overwhelming for patients and their loved ones. Here are some essential aspects to consider:
- Emotional Support: Patients and their families may benefit from seeking emotional support through counseling, support groups, or therapy to navigate the emotional challenges associated with a stage 4 cancer diagnosis.
- Pain Management: Managing pain and discomfort is crucial for patients with stage 4 pancreatic cancer. Healthcare providers can offer various pain management strategies, including medications, nerve blocks, and complementary therapies.
- Nutritional Support: Maintaining proper nutrition is essential for patients with advanced pancreatic cancer. Working with a registered dietitian can help ensure that patients receive adequate nutrition to support their overall well-being.
- Hospice Care: As the disease progresses, patients may consider hospice care to provide comfort and support in their final stages of life. Hospice services focus on enhancing quality of life and providing compassionate end-of-life care.
Seeking Support And Information
Receiving a diagnosis of stage 4 pancreatic cancer can be daunting, but seeking support and reliable information is crucial for patients and their families. It’s essential to connect with healthcare providers, seek second opinions, and explore available resources to make informed decisions about treatment and care.
Remember that each patient’s journey is unique, and accessing support and information can make a significant difference in their experience with stage 4 pancreatic cancer.
Is Pancreatic Cancer Hereditary
Pancreatic cancer can have a hereditary component, with some cases linked to genetic factors. Individuals with a family history of the disease may have a higher risk of developing pancreatic cancer. It is recommended for those with a family history to consult with a healthcare provider for proper evaluation and monitoring.
Is Pancreatic Cancer Hereditary?
Pancreatic cancer is a complex disease that can be influenced by genetic factors. Understanding the hereditary aspect of pancreatic cancer is crucial for individuals with a family history of the disease.
Genetic Risk Factors:
- Certain gene mutations, such as BRCA1, BRCA2, and PALB2, are associated with an increased risk of pancreatic cancer.
- Individuals with a family history of pancreatic cancer are at a higher risk of developing the disease.
Screening And Genetic Counseling:
- Genetic testing can help identify individuals with a higher genetic risk of pancreatic cancer.
- Genetic counseling can provide personalized risk assessment and guidance on screening options.
Lifestyle And Environmental Factors:
- While genetics play a role, lifestyle and environmental factors also contribute to the development of pancreatic cancer.
- Maintaining a healthy lifestyle, such as avoiding smoking and excessive alcohol consumption, can help reduce the risk.
Understanding the hereditary component of pancreatic cancer can help individuals make informed decisions about screening and risk management. Genetic counseling and testing are valuable tools in assessing and managing the risk of developing this challenging disease.
Pancreatic Cancer Symptoms Female
Pancreatic cancer symptoms in females may include dull or gnawing pain in the upper abdomen that can spread to the back. As the tumor progresses, the pain may become more constant and worsen after eating or lying down. Weight loss and abdominal pain are common in advanced stages of pancreatic cancer.
Understanding Pancreatic Cancer Symptoms In Females
Pancreatic cancer symptoms in females may differ slightly from those in males. It is crucial for women to be aware of the signs and symptoms of pancreatic cancer, as early detection can significantly impact treatment outcomes. Here are some important symptoms of pancreatic cancer in females to be mindful of:
Common Symptoms
- Abdominal pain: Women with pancreatic cancer may experience persistent pain in the upper abdomen that can radiate to the back.
- Jaundice: Yellowing of the skin and eyes can occur due to the obstruction of the bile duct by the growing tumor.
- Unexplained weight loss: Significant and unexplained weight loss can be a sign of pancreatic cancer.
- Loss of appetite: Many women with pancreatic cancer experience a sudden loss of appetite.
- Digestive problems: Symptoms such as nausea, vomiting, and changes in bowel movements can indicate pancreatic cancer.
It’s important to note that these symptoms can be caused by various health conditions, and experiencing them does not necessarily mean one has pancreatic cancer. However, if any of these symptoms persist or worsen, it is crucial to seek medical attention promptly.
Seeking Medical Advice
If a woman experiences any of the aforementioned symptoms persistently, it is essential to consult a healthcare professional for a thorough evaluation. Early detection and timely medical intervention play a vital role in improving the prognosis of pancreatic cancer.
Being vigilant about potential symptoms and seeking medical advice promptly can aid in the early detection and treatment of pancreatic cancer in females. It is important for women to be proactive about their health and not dismiss any concerning symptoms they may experience.
What Is Pancreatic Cancer
Pancreatic cancer is a type of cancer that affects the pancreas, a gland located in the abdomen that produces digestive enzymes and hormones that regulate blood sugar. Symptoms of pancreatic cancer include abdominal pain, weight loss, and jaundice. The disease is difficult to diagnose and treat, and has a low survival rate.
Understanding Pancreatic Cancer
Pancreatic cancer is a type of cancer that develops in the pancreas, a vital organ located behind the stomach. This disease occurs when abnormal cells in the pancreas grow uncontrollably, forming a tumor. Pancreatic cancer is known for its aggressive nature and often goes undetected until it reaches advanced stages.
Key Points About Pancreatic Cancer:
- Symptoms: Pancreatic cancer may initially present with vague symptoms such as abdominal pain, jaundice, weight loss, and digestive issues.
- Diagnosis: Detecting pancreatic cancer can be challenging due to its nonspecific symptoms. Imaging tests like ultrasound, CT scans, MRI scans, and PET scans are commonly used for diagnosis.
- Treatment: Treatment options for pancreatic cancer include surgery, chemotherapy, radiation therapy, and targeted therapy. The choice of treatment depends on the stage and type of pancreatic cancer.
- Prognosis: Pancreatic cancer has a low survival rate compared to other cancers due to its aggressive nature and late diagnosis. Early detection is crucial for improving outcomes.
Impact Of Pancreatic Cancer:
Pancreatic cancer can significantly impact a person’s quality of life and overall well-being. The physical and emotional toll of this disease can be challenging for both patients and their families. Seeking support from healthcare professionals and support groups is essential in managing the effects of pancreatic cancer.
Causes Of Pancreatic Cancer
Pancreatic cancer can be caused by genetic mutations, smoking, obesity, and family history. Early detection is crucial for treatment.
Pancreatic Cancer: Causes And Risk Factors
Pancreatic cancer is one of the most deadly forms of cancer, with a 5-year survival rate of only 10%. This type of cancer occurs when abnormal cells grow in the pancreas, a gland that produces enzymes to help with digestion and hormones to regulate blood sugar levels.
While the exact are not fully understood, there are several risk factors that increase the likelihood of developing this disease.
Genetics And Family History
In some cases, pancreatic cancer can be caused by inherited genetic mutations. Individuals with a family history of pancreatic cancer are at a higher risk of developing the disease themselves. In particular, mutations in the BRCA2 gene and the PALB2 gene have been linked to an increased risk of pancreatic cancer.
Age And Gender
The risk of developing pancreatic cancer increases with age, with most cases occurring in individuals over the age of 60. Men are also slightly more likely to develop pancreatic cancer than women.
Lifestyle Factors
Several lifestyle factors have been linked to an increased risk of pancreatic cancer, including:
- Smoking: Cigarette smoking is the most significant risk factor for pancreatic cancer, with smokers being two to three times more likely to develop the disease than non-smokers.
- Obesity: Individuals who are overweight or obese are at an increased risk of developing pancreatic cancer.
- Diabetes: People with diabetes are more likely to develop pancreatic cancer, although it is not yet clear whether diabetes causes pancreatic cancer or if the two conditions share common risk factors.
Other Risk Factors
Other factors that may increase the risk of pancreatic cancer include chronic pancreatitis (inflammation of the pancreas), exposure to certain chemicals and toxins, and a diet high in red meat and processed foods.
While it is not always possible to prevent pancreatic cancer, understanding the risk factors can help individuals take steps to reduce their risk. Quitting smoking, maintaining a healthy weight, and managing diabetes can all help lower the risk of developing pancreatic cancer.
Additionally, individuals with a family history of pancreatic cancer may benefit from genetic counseling and testing to identify any inherited mutations that may increase their risk.
Pancreatic Cancer Stage 4
Pancreatic cancer stage 4 is an advanced stage, often spreading to the liver, lymph nodes, abdomen, lungs, and sometimes, the bones. Symptoms may include weight loss and abdominal pain. The prognosis for stage 4 pancreatic cancer is often poor, but treatment options are available to manage symptoms and improve quality of life.
Understanding Pancreatic Cancer Stage 4
Pancreatic cancer stage 4 is the most advanced stage of pancreatic cancer, indicating that the cancer has spread to distant organs or tissues beyond the pancreas. At this stage, the cancer is typically considered inoperable and may present significant challenges in terms of treatment options and prognosis.
Symptoms Of Pancreatic Cancer Stage 4
- Jaundice: Yellowing of the skin and eyes due to bile duct obstruction.
- Weight loss: Unexplained and rapid weight loss.
- Severe abdominal pain: Persistent and severe pain in the abdomen.
- Fatigue: Overwhelming tiredness and lack of energy due to the cancer’s impact on the body.
- Digestive issues: Nausea, vomiting, and changes in bowel habits.
Treatment Options For Pancreatic Cancer Stage 4
- Chemotherapy: Administered to help shrink the tumor and alleviate symptoms.
- Radiation therapy: Used to target and destroy cancer cells.
- Palliative care: Focuses on improving quality of life and managing symptoms.
Prognosis And Challenges
- Poor prognosis: Pancreatic cancer stage 4 has a low survival rate.
- Metastasis: The cancer’s spread to distant sites makes treatment more challenging.
- Quality of life: Focus shifts to symptom management and comfort care.
Support And Resources
- Seek support from healthcare professionals, support groups, and online resources.
- Consider palliative care options for symptom management and emotional support.
Coping With Pancreatic Cancer Stage 4
- Maintain open communication with your healthcare team.
- Engage in activities that bring comfort and emotional support.
- Prioritize self-care and mental well-being during the treatment process.
Remember
Pancreatic cancer stage 4 presents significant challenges, but with the right support and treatment, managing symptoms and maintaining quality of life are achievable goals. Stay informed, seek support, and prioritize your well-being throughout the journey.
My First Symptoms Of Pancreatic Cancer
Experiencing a dull pain in the upper abdomen that may radiate to the back was among my first symptoms of pancreatic cancer. This discomfort can vary in intensity and frequency, often worsening with lying down or after meals. Early detection and timely treatment are crucial for managing this condition effectively.
- Sudden weight loss: Unexplained weight loss can be a common early sign of pancreatic cancer as the tumor affects the body’s ability to digest food properly.
- Jaundice: Yellowing of the skin and eyes may occur due to the blockage of the bile duct by the pancreatic tumor.
- Abdominal pain: Persistent pain in the upper abdomen or back that may worsen after eating is a symptom that should not be ignored.
- Changes in stool: Light-colored or greasy stools can indicate issues with the pancreas and digestion.
- Loss of appetite: A sudden decrease in appetite and feelings of fullness even after small meals can be a sign of pancreatic cancer.
Seeking Medical Attention
- Consult a healthcare provider: If you experience any of these symptoms persistently, it is crucial to seek medical advice promptly.
- Diagnostic tests: Your healthcare provider may recommend imaging tests such as ultrasound, CT scans, or MRI scans to investigate further.
- Blood tests: Specific blood tests can help detect markers associated with pancreatic cancer and aid in early diagnosis.
- Specialist consultation: Referral to a gastroenterologist or oncologist may be necessary for a comprehensive evaluation and treatment plan.
Taking Action
- Early detection is key: Pancreatic cancer is often diagnosed at an advanced stage, emphasizing the importance of recognizing symptoms early.
- Lifestyle modifications: Maintaining a healthy diet, regular exercise, and avoiding tobacco and excessive alcohol consumption can help reduce the risk of developing pancreatic cancer.
- Support system: Seek support from loved ones, support groups, or mental health professionals to navigate the emotional challenges that may arise during diagnosis and treatment.
- Stay informed: Educate yourself about pancreatic cancer, treatment options, and available resources to make informed decisions about your health.
Remember
Pancreatic cancer can present with vague symptoms that may mimic other conditions, making it crucial to pay attention to any persistent changes in your health. Early detection and timely medical intervention can significantly impact the outcome of pancreatic cancer treatment.
Prioritize your health and well-being by being proactive in addressing any concerning symptoms promptly.
What Are The Symptoms Of Pancreatic Cancer In A Woman?
Pancreatic cancer symptoms in women can include abdominal pain that may spread to the back, unexplained weight loss, jaundice, and digestive issues. These symptoms can be vague and easily overlooked, making early detection challenging. If experiencing any of these symptoms, it’s important to seek medical attention promptly for proper evaluation and diagnosis.
Pancreatic Cancer: What Are The Symptoms In Women?
Pancreatic cancer is a serious illness that affects both men and women. However, the symptoms of pancreatic cancer can vary depending on the individual. In this section, we will discuss the symptoms of pancreatic cancer in women.
Feeling
One of the most common symptoms of pancreatic cancer in women is a dull or gnawing pain in the upper part of the abdomen that may spread to the sides or back. This pain may come and go to begin with, but as the tumor becomes larger and more advanced, the pain may be more constant and last longer.
Some women may not experience any pain at all, but others may describe it as a dull or gnawing sensation.
Pain
Pancreatic cancer can also cause a dull pain in the upper tummy (abdomen) that may spread to the back. This pain is often worse when lying down or after eating. As the tumor grows, the pain may become more severe and last longer.
Other Symptoms
In addition to pain, there are other symptoms that women with pancreatic cancer may experience. These include:
- Jaundice (yellowing of the skin and eyes)
- Unexplained weight loss
- Loss of appetite
- Nausea and vomiting
- Fatigue
- Itchy skin
If you experience any of these symptoms, it is essential to speak with your doctor as soon as possible.
Diagnosis
If your doctor suspects that you may have pancreatic cancer, they will likely order a series of tests to diagnose the condition. These tests may include imaging tests like ultrasounds, CT scans, or MRI scans. In some cases, a biopsy may be necessary to confirm the diagnosis.
The symptoms of pancreatic cancer in women can vary, but they often include pain in the upper abdomen or back, jaundice, unexplained weight loss, and fatigue. If you experience any of these symptoms, it is crucial to speak with your doctor as soon as possible to receive a diagnosis and begin treatment.
Stage 2 Pancreatic Cancer
Stage 2 pancreatic cancer indicates the cancer has spread beyond the pancreas to nearby lymph nodes or blood vessels, but not to distant organs. Treatment may involve surgery, chemotherapy, or radiation therapy. The prognosis at this stage varies, and early detection is crucial for better outcomes.
Understanding Stage 2 Pancreatic Cancer:
- Stage 2 pancreatic cancer is characterized by the tumor being confined to the pancreas and potentially involving nearby lymph nodes.
- The cancer has not spread to distant organs at this stage, making treatment more feasible and offering a better prognosis.
- Patients with may experience symptoms such as abdominal pain, jaundice, weight loss, and digestive issues.
Treatment Options For Stage 2 Pancreatic Cancer:
- Surgery is a common treatment approach for stage 2 pancreatic cancer, aiming to remove the tumor and affected lymph nodes.
- Chemotherapy and radiation therapy may be used before or after surgery to shrink the tumor and target any remaining cancer cells.
- Clinical trials and targeted therapies are also being explored as potential treatment options for stage 2 pancreatic cancer patients.
Prognosis And Survival Rates For Stage 2 Pancreatic Cancer:
- The prognosis for stage 2 pancreatic cancer varies depending on factors such as the tumor size, location, and response to treatment.
- With advancements in treatment options and early detection, the survival rates for stage 2 pancreatic cancer have been improving.
- Regular follow-up care and monitoring are essential for stage 2 pancreatic cancer survivors to detect any recurrence or new developments early on.
How To Prevent Pancreatic Cancer
Preventing pancreatic cancer involves adopting a healthy lifestyle, such as maintaining a balanced diet, regular exercise, and avoiding tobacco and excessive alcohol. Additionally, staying at a healthy weight and managing chronic conditions like diabetes can reduce the risk of developing this disease.
Regular medical check-ups and screenings are also important for early detection and prevention.
Ways To Prevent Pancreatic Cancer
Pancreatic cancer is a serious disease with a low survival rate. While there are no guaranteed ways to prevent pancreatic cancer, there are several strategies that may lower the risk of developing this condition. Here are some important steps you can take to reduce your risk of pancreatic cancer:
- Maintain a Healthy Weight: Obesity has been linked to an increased risk of pancreatic cancer. By adopting a healthy diet and engaging in regular physical activity, you can maintain a healthy weight and lower your risk.
- Quit Smoking: Smoking is a major risk factor for pancreatic cancer. If you smoke, quitting can significantly reduce your risk of developing this disease.
- Limit Alcohol Consumption: Excessive alcohol consumption has been associated with an elevated risk of pancreatic cancer. Moderating your alcohol intake can help lower your risk.
- Eat a Balanced Diet: Consuming a diet rich in fruits, vegetables, and whole grains, while limiting red and processed meats, may help reduce the risk of pancreatic cancer.
- Manage Diabetes: Individuals with diabetes are at a higher risk of developing pancreatic cancer. Managing diabetes through proper medication, diet, and exercise can help lower the risk.
Importance Of Regular Medical Check-ups
Regular medical check-ups are crucial for early detection and treatment of any potential health issues, including pancreatic cancer. Here’s why regular check-ups are essential:
- Early Detection: Regular check-ups can help detect any abnormalities in the pancreas at an early stage, improving the chances of successful treatment.
- Risk Assessment: Healthcare professionals can assess your individual risk factors for pancreatic cancer and provide personalized recommendations for prevention and early detection.
- Health Monitoring: Routine check-ups allow for the monitoring of overall health, enabling early intervention if any concerning symptoms or risk factors are identified.
Taking proactive steps to maintain a healthy lifestyle and attending regular medical check-ups can play a vital role in reducing the risk of pancreatic cancer. While there are no foolproof methods for preventing this disease, these strategies can contribute to a lower risk and improved overall health.
What Are The Symptoms Of Pancreatic Cancer In A Woman?
Pancreatic cancer symptoms in women include abdominal pain that may spread to the back, weight loss, and digestive issues such as nausea and vomiting. Additionally, jaundice, changes in stool color, and diabetes can also be signs of pancreatic cancer. Early detection is crucial for effective treatment.
Symptoms Of Pancreatic Cancer In Women:
- Jaundice: Yellowing of the skin and whites of the eyes due to the buildup of bilirubin in the body.
- Abdominal Pain: Dull or sharp pain in the upper abdomen that may radiate to the back.
- Unexplained Weight Loss: Sudden and unexplained weight loss without changes in diet or exercise.
- Changes in Bowel Habits: Diarrhea, constipation, or changes in stool consistency may occur.
- Loss of Appetite: A decrease in appetite and feeling full quickly after eating.
Recognizing The Symptoms:
Women experiencing persistent symptoms such as jaundice or unexplained weight loss should seek medical evaluation promptly.
Understanding The Significance:
Early detection of pancreatic cancer symptoms in women can lead to timely diagnosis and improved treatment outcomes.
Seeking Medical Advice:
If you or a loved one are experiencing any of these symptoms, consult a healthcare provider for proper evaluation and diagnosis.
Promoting Awareness:
Educating women about the symptoms of pancreatic cancer can help in early detection and better prognosis.
What Are The Signs Of Pancreatic Cancer
Pancreatic cancer signs include abdominal pain, weight loss, jaundice, and digestive issues. Symptoms may vary, and early detection is crucial for treatment success.
Signs Of Pancreatic Cancer
Pancreatic cancer is often called a “silent disease” because it can be difficult to detect in its early stages. However, there are certain signs and symptoms that may indicate the presence of this condition. Being aware of these signs is crucial for timely diagnosis and treatment.
Symptoms To Look Out For
- Jaundice: This condition causes yellowing of the skin and the whites of the eyes due to the build-up of bilirubin in the body.
- Unexplained weight loss: Losing a significant amount of weight without trying could be a sign of pancreatic cancer.
- Abdominal pain: Discomfort or pain in the abdomen, particularly in the upper part, may be indicative of this condition.
- Changes in stool: Light-colored or greasy stools can be a result of pancreatic enzyme deficiency due to cancer.
These symptoms may not necessarily indicate pancreatic cancer, but if you experience any of them, it’s important to consult a healthcare professional for further evaluation.
What Does Pancreatic Cancer Feel Like
- Dull or gnawing pain: Many people describe the pain associated with pancreatic cancer as a dull or gnawing sensation in the upper abdomen that may spread to the back.
- Pain variability: Initially, the pain may come and go, but as the cancer progresses, it may become more constant and severe, especially after eating or lying down.
Being attuned to these sensations and seeking medical advice promptly can make a difference in the early detection and management of pancreatic cancer.
Early recognition of the signs and symptoms of pancreatic cancer is crucial for timely intervention. If you notice any of these symptoms, it is important to consult a healthcare professional for further evaluation and appropriate management.
Pancreatic Cancer Spread To Liver How Long To Live
Pancreatic cancer that has spread to the liver typically has a low survival rate, with a median life expectancy of around 3 to 6 months. However, individual outcomes may vary based on factors such as overall health and response to treatment.
It’s important for patients to consult with healthcare professionals for personalized prognosis and care options.
Understanding Pancreatic Cancer Spread To Liver How Long To Live
Pancreatic cancer, when it spreads to the liver, can significantly impact the prognosis and life expectancy of the patient. Here’s a look at the factors that influence how long a person may live after the cancer spreads to the liver:
Factors Affecting Life Expectancy
- Tumor Size and Location: The size and location of the pancreatic tumor and its spread to the liver play a crucial role in determining the life expectancy of the individual. Larger tumors and extensive liver involvement may lead to a shorter life expectancy.
- Treatment Response: The response to treatment, such as chemotherapy, radiation therapy, or surgery, can impact the progression of the cancer and, subsequently, the patient’s survival rate.
- Overall Health: The overall health and strength of the patient’s immune system can influence their ability to withstand the effects of the cancer and its treatment, thereby affecting their life expectancy.
- Metastasis Spread: The extent and speed of the cancer’s spread to the liver and other organs can also impact the prognosis and life expectancy of the individual.
Prognosis And Survival Rates
- The 5-year survival rate for pancreatic cancer that has spread to the liver is generally low, with only about 3% of patients surviving for 5 years or more after diagnosis.
- The median survival time for patients with advanced pancreatic cancer that has spread to the liver is typically around 6 months to a year.
Given the aggressive nature of pancreatic cancer and its impact when it spreads to the liver, it’s essential for patients and their families to seek support, stay informed about treatment options, and work closely with healthcare professionals to make well-informed decisions.
Seeking Support And Care
- Palliative Care: Patients with advanced pancreatic cancer, especially when it spreads to the liver, may benefit from palliative care services aimed at improving their quality of life and managing symptoms such as pain, nausea, and fatigue.
- Emotional Support: Coping with a diagnosis of pancreatic cancer and its spread to the liver can be emotionally challenging. Seeking support from friends, family, support groups, or mental health professionals can be beneficial for both the patient and their loved ones.
It’s important to remember that every individual’s situation is unique, and the information provided here serves as a general guide. Consulting with healthcare providers for personalized guidance and support is crucial in navigating the complexities of pancreatic cancer and its impact on life expectancy.
Frequently Asked Questions
What Is The Life Expectancy For Pancreatic Cancer?
The life expectancy for pancreatic cancer varies, with a five-year survival rate of around 10%.
Can Pancreatic Cancer Be Cured?
Pancreatic cancer cannot always be cured, but it can be treated. The treatment plan depends on the stage of the cancer and the overall health of the patient. Early detection and treatment offer the best chance for a positive outcome.
However, pancreatic cancer is a highly lethal disease and the long-term survival rate is low.
How Fast Does Pancreatic Cancer Progress?
Pancreatic cancer progresses rapidly, with some cases advancing in just a few months.
What Is The Longest Someone Has Survived Pancreatic Cancer?
The longest survival for pancreatic cancer is 20 years. It is exceptional but possible.
Conclusion
Pancreatic cancer is a devastating disease that affects many individuals and their families. It is important to be aware of the symptoms and risk factors associated with this disease, as early detection can greatly improve the chances of successful treatment.
While there is no cure for pancreatic cancer, there are treatments available that can improve quality of life and extend survival. If you or a loved one has been diagnosed with pancreatic cancer, it is important to seek out the guidance and support of healthcare professionals and loved ones.
Remember, you are not alone in this fight.