Supporting someone through a miscarriage is delicate, requiring empathy, understanding, and practical help. Here are 10 comprehensive ways to support someone experiencing a miscarriage:
1. Acknowledge the Loss
Miscarriage can be a deeply personal and painful experience. It’s essential to acknowledge the loss without diminishing its significance. Avoid saying things like “It was meant to be” or “At least it happened early.” Instead, simple statements like “I’m sorry for your loss” or “I’m here for you” can be much more comforting.
Key Points:
- Validate the grief, recognizing that a miscarriage is not “just” a medical event but often an emotional and psychological trauma.
- Avoid dismissive or minimizing statements, even if intended to provide comfort.
- Allow the person to express their grief in their own way—whether through talking, crying, or even silence.
2. Offer Emotional Support
Emotional support goes beyond just expressing sympathy. It involves being a consistent, compassionate presence in the person’s life. Be available to listen when they need to talk, and be respectful of their space if they need solitude.
Key Points:
- Let the grieving person lead the conversation, offering them space to share their feelings without rushing or directing the conversation.
- Offer a non-judgmental ear and avoid giving advice unless specifically asked.
- Respect their emotional timeline—grief from miscarriage doesn’t follow a set schedule, and some may need more time to process their feelings than others.
3. Avoid Platitudes
Common well-meaning statements can often cause more harm than good. Phrases like “It wasn’t meant to be” or “You can try again” may dismiss the gravity of the loss. It’s important to steer clear of platitudes, focusing instead on the individual’s emotions.
Key Points:
- Refrain from making comparisons, like discussing other people’s experiences or your own unless they specifically ask for it.
- Avoid trying to explain the miscarriage in spiritual or cosmic terms unless you are sure that aligns with the grieving person’s beliefs.
- Stick to phrases that communicate genuine empathy, like “I’m so sorry you’re going through this” or “I can’t imagine how difficult this must be.”
4. Give Practical Help
Miscarriage can take both a physical and emotional toll, leaving someone exhausted and in need of rest. Offering practical help can be invaluable during this time, as they might struggle to keep up with day-to-day tasks.
Key Points:
- Offer to help with meals, household chores, or caring for other children if applicable.
- Respect their autonomy—don’t force your help on them, but gently insist if you notice they need it.
- Sometimes, taking care of logistical matters like grocery shopping, paying bills, or doing laundry can give them space to focus on healing.
5. Respect Their Privacy
Not everyone feels comfortable sharing their miscarriage experience with others. Some may want to keep it private, while others may be open about their loss. It’s important to respect their wishes regarding who is informed and how they share their experience.
Key Points:
- Always ask before discussing their miscarriage with others, even mutual friends or family members.
- If they prefer to keep the situation private, honor that boundary and be discreet in your support.
- Be mindful that social media can be a sensitive space, so avoid mentioning the miscarriage in posts unless they have publicly acknowledged it themselves.
6. Be Patient with Their Grief
Grieving after a miscarriage can take time, and everyone handles it differently. Some may process it quickly, while others may experience prolonged periods of sorrow. Be patient with their journey and refrain from pushing them to “move on” or “get back to normal” prematurely.
Key Points:
- Understand that grief is non-linear; they may experience good days and bad days, even months or years after the event.
- Reassure them that it’s okay to grieve and that there’s no set timeline for when they should start feeling better.
- Check in regularly over time—people often offer support immediately after a loss but forget to do so in the weeks or months that follow.
7. Respect Their Physical Recovery
In addition to emotional healing, the person will also be recovering physically. Depending on the stage of the miscarriage and any medical procedures involved, they may be dealing with significant physical discomfort or fatigue.
Key Points:
- Ask how they’re feeling physically, but be sensitive—don’t push them to talk about their symptoms if they’re uncomfortable.
- Encourage rest and offer support for their physical needs, such as transportation to medical appointments or help with managing pain or discomfort.
- Remind them to follow up with their healthcare provider for post-miscarriage care, but do so gently, without making them feel pressured.
8. Offer Resources for Professional Support
Sometimes, professional guidance from a therapist or counselor trained in grief and loss can be incredibly beneficial. While you can be an emotional anchor, there may be times when your friend or loved one needs specialized support.
Key Points:
- Gently suggest resources for professional counseling or support groups, especially if the person seems to be struggling deeply with their emotions.
- Offer to help them find a therapist or accompany them to a session if they feel unsure about seeking help on their own.
- Be sensitive to the fact that not everyone is ready for professional help right away; provide the information and leave the decision up to them.
9. Understand Milestone Grief
Grief after a miscarriage doesn’t always fade with time—it can resurface during significant dates such as the due date, anniversaries, or holidays. Being mindful of these potential triggers can help you offer additional support when it’s needed most.
Key Points:
- If you’re close to the person, consider marking the baby’s due date on your calendar and checking in with them around that time.
- Acknowledge that milestone dates may be difficult, but avoid assuming or forcing the person to address them if they don’t want to.
- Be prepared to offer support during holidays or family gatherings, which can intensify feelings of loss.
10. Offer Long-Term Support
Miscarriage is not just a momentary loss but a life-altering experience that may have long-term emotional effects. Even as time passes, continue to check in, offer your support, and be there for your loved one. Grief doesn’t end quickly, and your long-term presence can be incredibly comforting.
Key Points:
- Continue to check in with them even months after the miscarriage, letting them know that it’s okay to still be grieving.
- Encourage them to talk about their emotions and the experience whenever they feel the need, without forcing them to relive the pain.
- Remind them that you’re available for support at any time, and don’t hesitate to offer help in practical ways, even after the initial wave of grief has passed.
By understanding these essential aspects of support, you can help someone navigate the difficult journey of miscarriage with empathy, respect, and genuine care.

Most women experience one miscarriage in their lifetime. Having two or more miscarriages in a row is classified as recurrent miscarriage.
Miscarriage is a heartbreaking event for many couples trying to conceive. Understanding the frequency of miscarriages can help ease anxiety and provide clarity. Statistically, 10-20% of known pregnancies end in miscarriage, especially in the first trimester. Factors like age, health conditions, and lifestyle choices can influence these rates.
Women often wonder how many miscarriages are typical and when to seek medical advice. Knowing the signs, symptoms, and potential causes can empower individuals on their fertility journey. Seeking support from healthcare professionals and support groups can help navigate this emotional experience. Understanding your body and seeking answers is crucial for future pregnancies.
Miscarriage
Miscarriage Statistics
Understanding miscarriage statistics helps many people deal with their experiences. Miscarriage is a common occurrence. Knowing how often it happens can provide comfort and clarity. It also sheds light on the emotional and physical aspects of pregnancy loss. Let’s explore miscarriage statistics to gain insights into this sensitive topic.
Common Rates
Miscarriage rates vary, but here are some key statistics:
- About 10-20% of known pregnancies end in miscarriage.
- For women under 35, the risk is around 15%.
- Women aged 35-45 face a miscarriage rate of 20-35%.
- Over age 45, the risk can exceed 50%.
Here’s a simple table showing miscarriage rates by age:
| Age Group | Miscarriage Rate |
|---|---|
| Under 35 | 15% |
| 35-40 | 20-30% |
| Over 40 | 35-50% |
These rates indicate that miscarriage is common. Many women experience it. Understanding these rates helps reduce feelings of isolation. Remember, you are not alone in this journey.
Factors Influencing Rates
Several factors can affect miscarriage rates. Here are some critical influences:
- Age: Older women face higher risks.
- Health Conditions: Disorders like diabetes or thyroid problems increase risks.
- Lifestyle Choices: Smoking, drinking, and drug use can lead to miscarriages.
- Genetic Factors: Abnormalities in chromosomes can cause loss.
Other factors include:
- Previous Miscarriages: Having one or more increases the chance of future losses.
- Stress: High levels of emotional stress can impact pregnancy.
- Obesity: Being overweight can raise miscarriage risks.
Understanding these factors is essential. They help in recognizing personal risks. Awareness can guide healthier choices and improve outcomes.
Types Of Miscarriages
Understanding miscarriages can be challenging. Many women wonder about the different types of miscarriages and how they can affect future pregnancies. Each type of miscarriage has its unique characteristics and implications. Knowing these types helps in understanding the journey of pregnancy loss.
Early Miscarriage
Early miscarriages happen within the first 12 weeks of pregnancy. They are the most common type. Around 10% to 20% of known pregnancies end in early miscarriage. Many women may not even realize they were pregnant. Some signs include:
- Heavy bleeding
- Severe cramping
- Passing tissue or clots
Early miscarriages can occur for various reasons. Some common causes include:
- Chromosomal abnormalities
- Hormonal imbalances
- Uterine abnormalities
Most women can have healthy pregnancies after an early miscarriage. The body often recovers quickly. It is essential to seek medical advice if you experience symptoms. Here is a quick table summarizing early miscarriage facts:
| Aspect | Details |
|---|---|
| Time Frame | Within 12 weeks |
| Occurrence Rate | 10% to 20% |
| Common Symptoms | Bleeding, cramping, tissue passing |
Late Miscarriage
Late miscarriages occur between 13 and 20 weeks of pregnancy. They are less common but can be more emotionally challenging. Late miscarriages happen in about 1% to 5% of pregnancies. Causes may vary and include:
- Uterine infections
- Cervical incompetence
- Chronic health issues
Women may notice signs like:
- Severe abdominal pain
- Heavy bleeding
- Fluid leaking
Late miscarriages often require medical attention. Women may need extra support during this time. Here’s a simple table for late miscarriage facts:
| Aspect | Details |
|---|---|
| Time Frame | 13 to 20 weeks |
| Occurrence Rate | 1% to 5% |
| Common Symptoms | Pain, bleeding, fluid leakage |
Understanding these types helps women and families cope better with the loss.
Causes Of Miscarriage
Miscarriage can be a painful experience for many. Understanding the causes helps in coping with the situation. Several factors contribute to miscarriage. Knowing these factors can help you and your healthcare provider make informed decisions. Genetic factors and health conditions play significant roles in miscarriage.
Genetic Factors
Genetic factors are among the most common reasons for miscarriage. Chromosomal abnormalities often lead to complications during pregnancy. These abnormalities can happen during the formation of the egg or sperm. They can also occur during fertilization. Here are some key points about genetic factors:
- Chromosomal Abnormalities: About 50% of miscarriages occur due to these issues.
- Parental Genetics: Both parents’ genes can influence the risk of miscarriage.
- Inheritable Conditions: Some genetic disorders can be passed down, increasing risks.
Here’s a simple table showing common chromosomal abnormalities:
| Abnormality | Description |
|---|---|
| Trisomy 21 | Down syndrome, leading to developmental issues. |
| Turner Syndrome | Missing or incomplete X chromosome in females. |
| Triploidy | Extra set of chromosomes, often fatal in early pregnancy. |
These genetic issues can lead to early pregnancy loss. Understanding these can help in future pregnancies.
Health Conditions
Health conditions also contribute to the risk of miscarriage. Many women have underlying health issues that may affect pregnancy. Here are some common health conditions linked to miscarriage:
- Diabetes: Poorly controlled diabetes can increase miscarriage risk.
- Thyroid Disorders: Both hyperthyroidism and hypothyroidism can affect pregnancy.
- Autoimmune Disorders: Conditions like lupus can lead to pregnancy complications.
Other significant health conditions include:
- Obesity
- High blood pressure
- Infections
Regular check-ups can help manage these health conditions. Staying healthy is crucial for a successful pregnancy. Consult with your doctor for personalized advice.
:max_bytes(150000):strip_icc()/Parents-Stocksy_txpda973ff4dEa300_Medium_3816428-052f0f3138e84f5bb613626bcfd1d47c.jpg)
Credit: www.parents.com
Symptoms To Watch
Understanding how many times you can experience a miscarriage is important. Knowing the symptoms to watch for can help you seek timely medical advice. Recognizing these signs can aid in your emotional and physical well-being. Early detection of symptoms can lead to better care and support.
Physical Signs
Physical symptoms of a miscarriage can vary. It’s essential to pay attention to any unusual changes in your body. Common physical signs include:
- Heavy bleeding: This may include passing clots or tissue.
- Severe abdominal pain: Cramping may feel intense and sharp.
- Back pain: Constant or severe pain may indicate a problem.
- Fluid discharge: Any unusual fluid release can be a red flag.
Tracking these signs can help you communicate effectively with your healthcare provider. Consider keeping a symptom diary. This can include:
| Date | Symptoms | Notes |
|---|---|---|
| 01/01 | Heavy bleeding | Lasted for 3 hours |
| 01/02 | Severe cramping | Pain level: 8/10 |
Being aware of these signs can help you act quickly. Don’t hesitate to contact a doctor if you notice anything unusual.
Emotional Signs
Experiencing a miscarriage can also affect your emotions. Many women feel a range of feelings that are completely normal. Watch for these emotional signs:
- Sadness: Feeling deeply sad is a common response.
- Anger: You may feel angry at yourself or the situation.
- Guilt: Many women blame themselves for the loss.
- Anxiety: Worrying about future pregnancies is common.
Talking about your feelings can be very helpful. Consider reaching out to friends or support groups. Writing in a journal can also assist in processing emotions. It’s essential to allow yourself to grieve.
Some women seek professional help. A therapist can provide tools to cope with loss. Remember, you are not alone in this journey.
Risk Factors
Understanding the risk factors associated with miscarriages is crucial for expectant parents. Many women experience pregnancy loss, and knowing the factors that can influence this can help with future pregnancies. This section will cover two main risk factors: age considerations and lifestyle factors. Each factor plays a significant role in the likelihood of having a miscarriage.
Age Considerations
Age is a vital factor in determining the risk of miscarriage. Women over the age of 35 face higher risks compared to younger women. This increase is due to various reasons, including genetic factors and overall health. Here are some key points:
- Women aged 20-30 have a 10-15% risk of miscarriage.
- Women aged 35-39 have a 20-35% risk.
- Women aged 40 and older can face a 40-50% risk.
Here’s a simple table to illustrate this:
| Age Group | Risk of Miscarriage |
|---|---|
| 20-30 years | 10-15% |
| 35-39 years | 20-35% |
| 40 years and older | 40-50% |
As women age, egg quality declines. This decline can lead to chromosomal abnormalities. Regular check-ups can help monitor health, especially as women approach their 30s and 40s.
Lifestyle Factors
Lifestyle choices significantly impact pregnancy health. Certain habits can increase the risk of miscarriage. Healthy lifestyle choices can lower this risk. Here are some common lifestyle factors:
- Smoking: Increases the risk by 30-40%.
- Excessive alcohol consumption: Linked to higher miscarriage rates.
- Obesity: Women with a high BMI are more likely to experience miscarriage.
- Poor nutrition: Lack of essential nutrients can affect pregnancy.
Maintaining a healthy lifestyle is essential. Here are some tips for a healthier pregnancy:
- Eat a balanced diet rich in fruits and vegetables.
- Exercise regularly with light activities.
- Avoid smoking and limit alcohol intake.
- Manage stress through relaxation techniques.
By focusing on these factors, women can improve their chances of a healthy pregnancy. Making positive changes can make a significant difference.

Credit: americanpregnancy.org
Frequency Of Miscarriages
Miscarriages can be a heartbreaking experience. Many women wonder about the frequency of miscarriages. Understanding how often they can happen is crucial for emotional and physical health. Miscarriages can occur once or multiple times. Each situation is unique. Recognizing the differences helps women and their families cope better.
One Vs. Multiple
One miscarriage is common and often happens without a clear reason. Many women recover well and go on to have healthy pregnancies. Here are some key points to understand:
- About 10-20% of known pregnancies end in miscarriage.
- Most women experience only one miscarriage in their lifetime.
- Many factors can contribute, like age and health conditions.
Multiple miscarriages are less common. If a woman has two or more miscarriages, it is termed “recurrent miscarriage.” Here’s a simple table showing the differences:
| Type | Description | Frequency |
|---|---|---|
| One Miscarriage | Single loss of pregnancy | Common |
| Multiple Miscarriages | Two or more consecutive losses | Less common |
Many women experience one miscarriage and go on to have healthy babies. Support from family and friends is vital during this time.
Recurrent Miscarriage
Recurrent miscarriage can be very distressing. It is defined as having three or more consecutive miscarriages. About 1% of women face this challenge. Understanding the causes can help manage expectations. Some common reasons include:
- Genetic issues in embryos.
- Hormonal imbalances.
- Uterine abnormalities.
Doctors often recommend tests after two miscarriages. Identifying issues can help in future pregnancies. Here’s a brief list of tests that may be conducted:
- Blood tests for hormonal levels.
- Genetic testing for parents.
- Ultrasound to check the uterus.
Support groups can provide emotional help. Many women find comfort in sharing their experiences. Education and support are essential for coping with recurrent miscarriages.
Medical Evaluation
Experiencing a miscarriage can be very difficult. Many women wonder how often it can happen. A medical evaluation can help answer these questions. It can identify any underlying health issues. Understanding your situation is essential for moving forward.
Tests Available
Medical evaluations often include various tests. These tests help determine the cause of repeated miscarriages. Here are some common tests:
- Blood Tests: Check hormone levels and immune system health.
- Karyotype Testing: Analyzes chromosomes for genetic issues.
- Ultrasound: Examines the uterus for abnormalities.
- Hysteroscopy: A procedure to look inside the uterus.
The following table summarizes key tests and their purposes:
| Test | Purpose |
|---|---|
| Blood Tests | Evaluate hormone levels |
| Karyotype Testing | Identify genetic problems |
| Ultrasound | Check for uterine abnormalities |
| Hysteroscopy | Inspect the uterus |
These tests provide valuable information. They help doctors understand why miscarriages happen. Each woman’s situation is unique. Tailored tests can lead to better outcomes.
Consulting Specialists
After initial tests, consulting specialists is important. They have expertise in reproductive health. A specialist can provide deeper insights into your condition. Here are some types of specialists to consider:
- Obstetricians: Focus on pregnancy and childbirth.
- Reproductive Endocrinologists: Experts in hormonal issues.
- Genetic Counselors: Help understand genetic risks.
- Maternal-Fetal Medicine Specialists: Deal with high-risk pregnancies.
Visiting these experts can provide:
- Detailed evaluations of your health.
- Personalized treatment plans.
- Support for emotional challenges.
Finding the right specialist can make a difference. They can offer hope and solutions. Do not hesitate to seek help. Your health and future pregnancies matter.
Emotional Impact
The journey through miscarriage can be deeply painful and challenging. Understanding the emotional impact is crucial for healing. Each loss brings a wave of feelings, such as sadness, anger, and confusion. These emotions can linger, making it hard to cope. Recognizing these feelings is the first step toward recovery. Support and effective coping mechanisms play a vital role in navigating this difficult time.
Coping Mechanisms
Finding ways to cope with the emotional pain of miscarriage is essential. Here are some effective strategies:
- Talk About It: Share feelings with friends or family.
- Journaling: Write down thoughts and emotions. This can help process feelings.
- Art Therapy: Express feelings through painting or drawing.
- Mindfulness: Practice meditation to find peace.
Creating a list of your feelings can also be beneficial:
| Emotion | How to Cope |
|---|---|
| Sadness | Talk to someone you trust. |
| Anger | Exercise or engage in a hobby. |
| Isolation | Join a support group. |
Each person copes differently. Try different methods to find what works best for you. It’s important to be gentle with yourself during this time.
Support Systems
Having a strong support system is vital after a miscarriage. Friends, family, and professionals can help. Here’s how to build your support network:
- Friends and Family: Lean on those who care about you. Share your feelings openly.
- Support Groups: Join groups for those who have experienced similar losses. You are not alone.
- Therapists: Professional help can guide you through grief.
Consider these benefits of support systems:
| Support Type | Benefits |
|---|---|
| Friends | Emotional comfort and understanding. |
| Support Groups | Shared experiences and encouragement. |
| Therapists | Professional advice and coping strategies. |
Open communication with your support network is key. Let them know how you feel and what you need. Their presence can provide comfort during this difficult time.
Future Pregnancies
Many people wonder about the effects of miscarriage on future pregnancies. Miscarriage can bring emotional and physical challenges. Understanding what comes next is vital. Many women successfully have healthy pregnancies after experiencing miscarriage. Knowing how to prepare is key.
Planning Ahead
Planning for future pregnancies can help ease worries. A few important steps can make a big difference:
- Understand Your Cycle: Track your menstrual cycle. This helps identify the best time to conceive.
- Healthy Lifestyle: Focus on nutrition, exercise, and avoiding harmful substances.
- Emotional Readiness: Consider your emotional state. Support from friends and family matters.
Here’s a simple table to summarize essential planning tips:
| Step | Description |
|---|---|
| Track Cycle | Monitor your menstrual cycle for better timing. |
| Nutrition | Eat healthy foods rich in vitamins and minerals. |
| Exercise | Stay active with regular, moderate exercise. |
| Support | Engage with supportive friends and family. |
Taking these steps can empower you. It can also help you feel more in control.
Consulting Healthcare Providers
Always talk to healthcare providers about future pregnancies. They can offer valuable insights and support. Regular check-ups are essential. Here’s why:
- Assess Health: Doctors can evaluate your overall health.
- Identify Risks: They help identify any risks for future pregnancies.
- Personalized Advice: Receive advice tailored to your medical history.
- Emotional Support: Providers can connect you with counseling services.
Consider these questions for your healthcare provider:
- What are my risks for future miscarriages?
- What tests can I take to understand my health better?
- How can I increase my chances of a healthy pregnancy?
- What support services are available if I need them?
These discussions can provide clarity. They can also reduce anxiety about future pregnancies.
Lifestyle Changes
Facing the question of how many times one can have a miscarriage can be daunting. Many women wonder about the impact of lifestyle changes on their reproductive health. Making positive lifestyle choices can help improve overall well-being. This can also reduce the risk of miscarriage. Knowing how to make these changes is essential for hopeful parents.
Healthy Habits
Adopting healthy habits can greatly enhance your chances of a successful pregnancy. Focus on nutrition, exercise, and mental health. Here are some vital components:
- Balanced Diet: Include fruits, vegetables, whole grains, and lean proteins.
- Regular Exercise: Aim for at least 30 minutes of moderate activity most days.
- Stay Hydrated: Drink plenty of water throughout the day.
- Adequate Sleep: Aim for 7-9 hours of quality sleep each night.
- Stress Management: Practice meditation or yoga to reduce stress levels.
Here’s a quick look at foods to include in your diet:
| Food Group | Examples |
|---|---|
| Fruits | Bananas, Berries, Apples |
| Vegetables | Spinach, Broccoli, Carrots |
| Proteins | Chicken, Fish, Lentils |
| Whole Grains | Brown Rice, Quinoa, Oats |
Integrating these habits into your daily routine is simple. Start small and gradually increase your efforts. Consistency is key for long-term benefits.
Avoiding Risks
Reducing risks is crucial for maintaining a healthy pregnancy. Several factors can contribute to miscarriage. Here are common risks to avoid:
- Tobacco Use: Smoking can harm your reproductive system.
- Alcohol Consumption: Even small amounts can affect fetal development.
- Illegal Drugs: Substances like cocaine and heroin can lead to complications.
- Excessive Caffeine: Limit intake to 200 mg per day.
- Environmental Toxins: Avoid exposure to harmful chemicals.
Be mindful of your surroundings and choices. Here are simple steps to minimize risks:
- Choose organic foods to reduce pesticide exposure.
- Use natural cleaning products.
- Avoid processed foods high in additives.
Making these adjustments can significantly lower the chances of miscarriage. Stay informed and proactive about your health.
Role Of Genetics
Many women wonder about the chances of having multiple miscarriages. Genetics play a significant role in this issue. Understanding how inherited traits can affect pregnancy is essential. Some genetic factors can increase the risk of miscarriage, making it vital to explore these aspects.
Inherited Conditions
Some inherited genetic conditions can lead to miscarriages. These conditions may affect the health of the embryo or fetus. Here are a few key points:
- Chromosomal Abnormalities: These are the most common causes of miscarriage. They occur when there are too many or too few chromosomes.
- Single Gene Disorders: Conditions like cystic fibrosis or sickle cell disease can affect pregnancy outcomes.
- Thrombophilia: This blood clotting disorder can disrupt blood flow to the placenta.
Some inherited conditions can be identified through family history. Genetic counseling can help assess risks. Here’s a simple table to summarize some inherited conditions:
| Condition | Effect on Pregnancy |
|---|---|
| Chromosomal Abnormalities | High risk of miscarriage |
| Single Gene Disorders | Possible complications |
| Thrombophilia | May lead to miscarriage |
Understanding these conditions can help women make informed choices. Genetic factors are just one piece of the puzzle.
Genetic Testing
Genetic testing can provide valuable insights for women with a history of miscarriage. This testing examines DNA for specific genetic mutations. Here are the benefits of genetic testing:
- Identifies Risks: Testing helps identify genetic conditions that may cause miscarriage.
- Guides Treatment: Knowing genetic factors can guide treatment options for future pregnancies.
- Supports Family Planning: Test results can help families make informed decisions about having children.
Common types of genetic tests include:
- Carrier Screening: Determines if parents carry genes for specific genetic disorders.
- Preimplantation Genetic Testing (PGT): Tests embryos for genetic conditions before implantation.
- Non-invasive Prenatal Testing (NIPT): Screens for chromosomal abnormalities during pregnancy.
Discussing genetic testing with a healthcare provider is essential. They can help interpret results and recommend the next steps. Knowledge of genetics can empower women facing multiple miscarriages.
Coping With Loss
Experiencing a miscarriage is a profound loss. Many people wonder how to cope with this heartache. Understanding the grieving process is crucial. Finding closure helps in healing. Each person’s journey through loss is unique. Support is essential during this time.
Grieving Process
The grieving process after a miscarriage can be overwhelming. Feelings of sadness, anger, and confusion are common. It’s important to allow yourself to feel these emotions. Here are some important aspects of the grieving process:
- Emotional Waves: Emotions may change from one moment to the next.
- Physical Reactions: Grief can cause fatigue, headaches, or even physical pain.
- Social Impact: Relationships may feel strained during this time.
Understanding the stages of grief can help:
| Stage | Description |
|---|---|
| Denial | A feeling of disbelief about the loss. |
| Anger | Frustration and resentment about the situation. |
| Bargaining | Thinking about what could have been done differently. |
| Depression | Deep sadness and withdrawal from life. |
| Acceptance | Finding peace with the loss. |
Talk to friends or family about your feelings. Consider joining a support group. Sharing your story can ease the burden. Remember, it’s okay to grieve in your own way.
Finding Closure
Finding closure after a miscarriage can be challenging. It involves emotional healing and acceptance. Here are some steps to help you find closure:
- Memorialize Your Loss: Create a small memorial for your baby.
- Write a Letter: Express your feelings in a letter to your baby.
- Seek Professional Help: A therapist can provide guidance through grief.
Consider these activities for closure:
- Plant a tree or flower in memory of your baby.
- Light a candle on special dates.
- Participate in remembrance events.
Closure takes time. Be gentle with yourself. Surround yourself with supportive people. Healing may come in waves, and that’s okay. Take each day as it comes.
Alternative Therapies
Many women face the heartache of miscarriage. Understanding how many times this can happen is important. Alternative therapies can help support emotional and physical well-being. These therapies may offer comfort and healing during difficult times.
Acupuncture
Acupuncture is an ancient Chinese therapy. It involves inserting thin needles into specific points on the body. Many women find it helps balance hormones and improve overall health. Studies show acupuncture may enhance fertility and reduce stress.
Here are some benefits of acupuncture:
- Reduces stress: Helps calm the mind and body.
- Improves blood flow: Enhances circulation to the reproductive organs.
- Balances hormones: Aids in regulating menstrual cycles.
- Supports emotional health: Can ease anxiety and depression.
Consider these points before starting acupuncture:
| Consideration | Details |
|---|---|
| Find a licensed acupuncturist | Ensure they specialize in women’s health. |
| Discuss with your doctor | Always consult your healthcare provider first. |
| Frequency of sessions | Regular visits may enhance benefits. |
Herbal Remedies
Herbal remedies have been used for centuries. They can support women’s health in various ways. Some herbs may help strengthen the body and improve fertility. Always consult a healthcare provider before trying herbal treatments.
Common herbs that support reproductive health include:
- Red Clover: Rich in nutrients, may balance hormones.
- Chaste Tree Berry: Helps regulate menstrual cycles.
- Ginger: Reduces inflammation and supports digestion.
- Raspberry Leaf: Strengthens the uterine muscles.
Important tips for using herbal remedies:
- Always research herbs thoroughly.
- Start with small doses.
- Monitor for side effects.
- Consult with a qualified herbalist or doctor.
Community Support
Miscarriages can be very hard. Many people feel alone during this time. Community support can make a big difference. Finding others who understand can help you heal. Connecting with groups and local resources offers comfort and strength.
Online Groups
Online support groups offer a safe space for those who have experienced miscarriages. They allow people to share their stories and feelings. Here are some benefits of joining these groups:
- 24/7 availability to talk
- Anonymity for privacy
- A diverse range of experiences
- Access to helpful resources
Many platforms host these groups. Here are some popular ones:
| Platform | Group Name | Focus Area |
|---|---|---|
| Miscarriage Support Group | General support and sharing | |
| r/Miscarriage | Community discussions | |
| What to Expect | Miscarriage Support | Advice and coping strategies |
People in these groups share coping tips and personal stories. It helps to know you are not alone. Support from others can ease the pain and guide you through tough times.
Local Resources
Local resources provide in-person support and connection. Many communities have groups for those who have faced miscarriage. Here are some types of local resources you might find:
- Support groups at hospitals
- Counseling services
- Workshops and seminars
- Community health centers
Here are some ways to find local resources:
- Ask your doctor for recommendations.
- Check with local hospitals or clinics.
- Look for community bulletin boards.
Many local support groups focus on sharing and healing. They create a sense of community. Being with others who understand can help you process your feelings. Remember, you are not alone in this journey.
When To Seek Help
Experiencing a miscarriage is a heartbreaking event. Many women wonder how many times they can go through this painful experience. Understanding when to seek help can make a big difference. It’s crucial to recognize signs of emotional distress and to know when professional support is needed.
Signs Of Distress
After a miscarriage, feelings of sadness and grief are normal. However, some signs may indicate deeper emotional distress. Recognizing these signs early can help you seek support.
- Persistent Sadness: Feeling sad most of the time.
- Withdrawal: Isolating yourself from family and friends.
- Anger or Irritability: Increased frustration over small issues.
- Sleep Issues: Trouble sleeping or sleeping too much.
- Loss of Interest: Not enjoying activities you once loved.
It’s also important to monitor physical symptoms. Emotional pain can sometimes lead to physical issues. Here’s a simple table to highlight signs to watch for:
| Physical Symptoms | Emotional Symptoms |
|---|---|
| Fatigue | Extreme sadness |
| Headaches | Feeling overwhelmed |
| Changes in appetite | Anxiety |
Recognizing these signs is essential. They might mean it’s time to reach out for help.
Consulting A Therapist
Seeing a therapist can be beneficial after experiencing a miscarriage. Therapy provides a safe space to express feelings. It helps in processing grief and finding coping strategies.
- Identify Feelings: A therapist can help you understand your emotions.
- Develop Coping Strategies: Learn ways to manage your grief.
- Improve Communication: Therapy can enhance how you talk about your feelings with loved ones.
Many types of therapy can help, such as:
- Cognitive Behavioral Therapy (CBT)
- Group Therapy
- Art or Music Therapy
Finding the right therapist is key. Look for someone experienced in dealing with pregnancy loss. A supportive therapist can guide you through this tough time.
Insurance Considerations
Understanding how many times a person can have a miscarriage is crucial for emotional and physical health. Insurance considerations play a key role in this journey. Many individuals may not know what their insurance covers. This can impact decisions about testing and treatment after multiple miscarriages.
Coverage For Testing
Insurance coverage for testing after a miscarriage varies widely. Many policies include some testing, but it’s not always complete. Understanding what tests are available can help you make informed decisions.
Common tests include:
- Karyotyping: A genetic test to check for chromosomal issues.
- Hysterosalpingography: An X-ray to see if the fallopian tubes are open.
- Thyroid function tests: To check if thyroid issues are affecting pregnancy.
It’s important to check your specific policy details. Some key points to consider:
| Test | Commonly Covered? | Notes |
|---|---|---|
| Karyotyping | Yes | May require prior authorization. |
| Hysterosalpingography | Sometimes | Check for specific criteria. |
| Thyroid tests | Usually | Coverage may depend on symptoms. |
Consult your healthcare provider and insurance company for the most accurate information. They can help clarify what is covered and what is not.
Costs Of Treatment
The costs associated with treatment after a miscarriage can be significant. Many couples face financial stress during this time. Understanding potential costs can help you plan better.
Common treatment options include:
- Medications: To address hormonal imbalances.
- Surgery: If there are structural issues in the uterus.
- Fertility treatments: Such as IVF or IUI.
Here are some estimated costs associated with these treatments:
| Treatment | Estimated Cost |
|---|---|
| Medications | $50 – $300 |
| Surgery | $3,000 – $10,000 |
| Fertility treatments | $12,000 – $15,000 |
Insurance may cover some of these costs, but it’s essential to verify your policy. Speak to your insurance provider for detailed information.
Pregnancy After Miscarriage
Many women wonder about the possibility of getting pregnant after a miscarriage. Miscarriages can be heartbreaking experiences. Each woman’s journey is unique. Understanding the right timing and emotional readiness is essential for a healthy pregnancy.
Timing Matters
After a miscarriage, the timing for trying again is crucial. The body needs time to heal. Experts suggest waiting at least one to three menstrual cycles before conceiving again. This allows for physical and emotional recovery. Here are some key points to consider:
- Physical Recovery: Your body needs time to regain strength.
- Menstrual Cycle: Regular cycles can help track ovulation.
- Doctor’s Advice: Always consult your healthcare provider.
Different women may have different recovery times. A table can help summarize the average recovery times:
| Recovery Period | Recommendation |
|---|---|
| 1 Month | Consider trying again if feeling ready. |
| 2-3 Months | Recommended time for most women. |
| Longer Than 3 Months | Seek medical advice for concerns. |
Every situation is different. Listen to your body and mind. Waiting for the right time is important for a healthy pregnancy.
Emotional Readiness
Emotional readiness is just as vital as physical health. Experiencing a miscarriage can lead to feelings of grief and anxiety. Taking the time to heal emotionally can improve chances for a successful pregnancy. Consider the following:
- Grief Process: Allow time to grieve the loss.
- Support Systems: Talk to friends, family, or support groups.
- Therapy: Professional help can be beneficial.
Ask yourself these questions to assess emotional readiness:
- Am I still grieving the loss?
- Do I feel hopeful about a new pregnancy?
- Can I manage stress during pregnancy?
Each woman’s emotional journey is unique. Taking time to heal can lead to a healthier mindset. A strong emotional foundation can help during the next pregnancy.

Credit: www.marchofdimes.org
Monitoring Health
Understanding how many times you can experience a miscarriage is crucial for your health. Monitoring health plays a vital role in this process. Regular doctor visits and being aware of your body can help you navigate this journey. Staying informed empowers you to seek help when needed.
Regular Check-ups
Regular check-ups with your healthcare provider are essential. These visits allow for open discussions about your health history and concerns. They help identify potential issues early on. Here are some key reasons why regular check-ups matter:
- Early Detection: Catch issues before they become serious.
- Personalized Care: Tailor your care based on your history.
- Emotional Support: Receive guidance and reassurance.
- Monitoring Progress: Track any changes in your health.
It’s advisable to schedule check-ups:
- Before trying to conceive.
- After a miscarriage.
- Every few months if trying again.
During these visits, your doctor may conduct tests. These can include blood tests and ultrasounds. A table below summarizes common tests:
| Test | Purpose |
|---|---|
| Blood Tests | Check hormone levels. |
| Ultrasound | Monitor fetal development. |
| Genetic Testing | Identify genetic issues. |
Tracking Symptoms
Tracking your symptoms can provide valuable insights into your health. Keeping a symptom diary is a great way to stay informed. This helps you share important information with your doctor during visits. Here’s how to track effectively:
- Note Physical Changes: Record any unusual pain or bleeding.
- Monitor Emotional Health: Write down your feelings and mood changes.
- Document Cycle Changes: Keep track of your menstrual cycle.
- Record Medications: List any medications you take.
Using a simple table can help you stay organized:
| Date | Symptoms | Notes |
|---|---|---|
| MM/DD/YYYY | Example: Cramps | Example: Mild, lasted 2 days |
| MM/DD/YYYY | Example: Spotting | Example: Light, for 1 day |
Being proactive about your health helps you feel empowered. It gives you a clearer picture of your body. Stay vigilant and engaged in your health journey.
Educating Yourself
Understanding how many times a person can have a miscarriage is vital. Educating yourself helps you deal with emotions and seeks the right support. Knowledge can empower you to make informed choices. It also aids in understanding your body better during this tough time.
Resources Available
Many resources can provide you with valuable information about miscarriages. These resources help in understanding potential causes and emotional impacts. Here are some useful options:
- Support Groups: Connect with others who share similar experiences.
- Online Forums: Engage in discussions and ask questions anonymously.
- Healthcare Providers: Consult doctors and specialists for personalized advice.
- Counseling Services: Seek professional help to manage grief and anxiety.
Consider looking for local and online resources. They can offer emotional and practical support. Here is a simple table of common resources:
| Type of Resource | Examples |
|---|---|
| Support Groups | Miscarriage Association, Resolve |
| Online Forums | BabyCenter, WhatToExpect |
| Healthcare Providers | Obstetricians, Midwives |
| Counseling Services | Therapists, Grief Counselors |
Using these resources can provide support and information. They can help you feel less alone during this difficult time.
Books And Articles
Books and articles offer in-depth knowledge about miscarriages. They cover various aspects, including emotional healing and physical health. Here are some recommended reads:
- “Miscarriage: A Shattered Dream” by Dr. Mike. This book discusses physical and emotional challenges.
- “The Miscarriage Support Handbook” by Sarah. It offers practical advice for coping.
- Articles from Medical Journals: They provide research on miscarriage causes and statistics.
Reading personal stories can also be comforting. It helps to know others have gone through similar experiences. Here are some article topics you might find helpful:
- Understanding the Causes of Miscarriage
- Emotional Effects of Miscarriage
- How to Talk About Your Loss
Gathering information from these books and articles can help you navigate this journey. Knowledge empowers you to take care of yourself better.
Sharing Your Story
Experiencing a miscarriage is a painful journey. Many people wonder, “How many times can you have a miscarriage?” Sharing your story can help you heal and connect with others. Talking about your experiences brings comfort and understanding. It shows you are not alone. Your story can inspire others facing similar challenges.
Empowerment Through Sharing
Sharing your story about miscarriage offers empowerment. It helps you process emotions. Many find comfort in knowing others understand their pain. Here are some benefits of sharing your experience:
- Reduces feelings of isolation
- Encourages open conversations
- Builds a support network
- Inspires others to share
Talking about your story can create a ripple effect. It encourages others to speak up. This can lead to a community of support. Here’s a table showing how sharing impacts others:
| Impact | Details |
|---|---|
| Emotional Healing | Sharing helps in processing grief. |
| Awareness | Increases understanding of miscarriage. |
| Connection | Builds relationships with those who relate. |
Empowerment through sharing can lead to healing. It allows your voice to be heard. You can transform your pain into hope for others.
Writing And Blogging
Writing about your experience can be therapeutic. Blogging allows you to express feelings freely. You can share insights and lessons learned. Here are some tips for writing your story:
- Be honest about your feelings.
- Describe your journey in detail.
- Include what helped you cope.
- Encourage others to share their stories.
Blogging also connects you with a wider audience. Here are ways to find your audience:
- Use social media platforms.
- Join support groups online.
- Engage with other bloggers.
Sharing your story through writing can create a safe space. This encourages others to open up. It can transform your pain into powerful messages. Your blog may become a beacon of hope for many.
Understanding Your Body
Understanding your body is key to navigating the journey of pregnancy. Many women wonder about the number of miscarriages they can experience. Miscarriages can be emotional and confusing. Knowing how your body works can help you feel more in control. Let’s explore the menstrual cycle and ovulation to gain insights into this important topic.
Menstrual Cycle Insights
The menstrual cycle plays a crucial role in female reproduction. It typically lasts about 28 days, but can vary. Understanding the phases of your cycle helps you recognize how your body prepares for pregnancy.
- Menstrual Phase: Days 1-5. The body sheds the uterine lining.
- Follicular Phase: Days 6-14. The body prepares an egg for release.
- Ovulation Phase: Day 14. The mature egg is released.
- Luteal Phase: Days 15-28. The body prepares for a possible pregnancy.
Each cycle is a chance for conception. It is important to track your cycle. This can help identify any irregularities. Here’s a simple table to show the average cycle length:
| Phase | Duration (Days) |
|---|---|
| Menstrual | 1-5 |
| Follicular | 6-14 |
| Ovulation | 14 |
| Luteal | 15-28 |
Recognizing these phases can help you understand your body better. If you notice irregularities, consult a healthcare provider. They can provide guidance and support.
Ovulation Awareness
Ovulation is a key event in the menstrual cycle. It is when an egg is released from the ovary. This usually occurs around day 14 of a 28-day cycle. Tracking ovulation can help in planning or preventing pregnancy.
Signs of ovulation include:
- Change in cervical mucus: It becomes clear and stretchy.
- Increased basal body temperature: A slight rise indicates ovulation.
- Ovulation pain: Some women feel slight discomfort.
Understanding your ovulation can help you identify fertile days. This is vital for women trying to conceive. Here’s a simple list to track your ovulation:
- Track your menstrual cycle.
- Look for changes in mucus.
- Measure your temperature daily.
- Note any pain or discomfort.
By being aware of ovulation, you can make informed decisions. This knowledge empowers women in their reproductive health journey.
Frequently Asked Questions
How Common Are Multiple Miscarriages?
Multiple miscarriages affect about 1-2% of women. While experiencing one miscarriage is common, two or more can indicate underlying issues. Factors may include genetic abnormalities, hormonal imbalances, or anatomical concerns. It’s essential to consult a healthcare professional for evaluation and support if multiple miscarriages occur.
What Are The Causes Of Repeated Miscarriages?
Repeated miscarriages can stem from various causes. Genetic factors, hormonal issues, and uterine abnormalities are common contributors. Autoimmune disorders and blood clotting disorders may also play a role. Consulting a healthcare provider can help identify the specific cause and guide appropriate treatment options.
Can Lifestyle Affect Miscarriage Rates?
Yes, lifestyle can significantly impact miscarriage rates. Factors like smoking, excessive alcohol, and poor diet can increase risks. Maintaining a healthy weight and managing stress levels are vital for reproductive health. Engaging in regular exercise and seeking medical advice can also support a healthier pregnancy journey.
How Can I Prevent Future Miscarriages?
While not all miscarriages can be prevented, some steps can help. Maintaining a balanced diet, managing stress, and avoiding harmful substances are crucial. Regular check-ups with a healthcare provider can identify and address underlying issues. Following medical advice during pregnancy can also improve outcomes.
Conclusion
Experiencing multiple miscarriages can be deeply challenging. Understanding the possible causes is crucial for your emotional and physical health. Seeking support from healthcare professionals can provide clarity and guidance. Remember, you’re not alone in this journey, and many resources are available to help you navigate these difficult times.
Can I Get Pregnant After 3 Miscarriages?
Yes, it is possible to get pregnant after three miscarriages. Many women go on to have successful pregnancies following multiple losses.
Experiencing three miscarriages can be emotionally and physically challenging. Women often worry about their chances of future pregnancies. Understanding the underlying causes of miscarriages can provide clarity. Factors like age, genetics, and health conditions play significant roles. Seeking medical advice is crucial for personalized guidance and support.
A healthcare provider can suggest tests to identify any issues. Many women achieve healthy pregnancies after miscarriages with the right care. Emotional support also remains essential during this journey. Knowing that others have successfully navigated this path can offer hope. Staying informed and proactive about reproductive health fosters confidence and resilience in future attempts to conceive.

Credit: www.news-medical.net
Pregnancy After Miscarriage
Many women wonder, Can I get pregnant after 3 miscarriages? The journey to pregnancy can be hard, especially after facing loss. Pregnancy after miscarriage is possible, but it often comes with emotional and physical challenges. Understanding these factors can help you prepare for a new pregnancy.
Emotional Impact
Experiencing a miscarriage is deeply emotional. After three losses, feelings of sadness, anxiety, and fear can intensify. It’s normal to have mixed emotions about trying again. Here are some common feelings:
- Grief: Mourning the loss of the expected baby.
- Anxiety: Worrying about future pregnancies.
- Guilt: Questioning if you did something wrong.
- Hope: Wanting to try for a healthy pregnancy.
Support is crucial during this time. Seeking help from friends, family, or professionals can be beneficial. A therapist can provide coping strategies. Joining support groups allows sharing experiences with others who understand.
| Feelings | How to Cope |
|---|---|
| Grief | Talk about your feelings. |
| Anxiety | Practice relaxation techniques. |
| Guilt | Remind yourself it’s not your fault. |
| Hope | Focus on positive outcomes. |
Take your time to heal emotionally. Each person’s journey is unique. Allow yourself to feel and process these emotions.
Physical Considerations
Physical health plays a key role in pregnancy after miscarriage. After three losses, it’s important to consult a healthcare provider. They can help assess your health and readiness. Here are some factors to consider:
- Medical Evaluation: Check for underlying health issues.
- Nutrition: Eat a balanced diet to support pregnancy.
- Exercise: Stay active but avoid strenuous activities.
- Weight Management: Maintain a healthy weight for pregnancy.
Regular check-ups help monitor your health. Your doctor may recommend tests to identify any problems. A healthy lifestyle can improve your chances of a successful pregnancy.
| Health Factor | Importance |
|---|---|
| Medical Evaluation | Identifies risks for future pregnancies. |
| Nutrition | Supports fetal development. |
| Exercise | Improves physical fitness. |
| Weight Management | Reduces complications during pregnancy. |
Focus on your overall health. It can make a big difference in your next pregnancy.
Understanding Miscarriages
Understanding miscarriages is essential for anyone facing pregnancy loss. Many women experience this heartbreaking event. After three miscarriages, the question arises: Can I get pregnant again? Knowing more about miscarriages can help you navigate your feelings and future pregnancies. This section will explore the types of miscarriages and their common causes.
Types Of Miscarriages
Miscarriages can occur in various forms. Each type has different signs and implications. Here are the main types of miscarriages:
- Threatened Miscarriage: Bleeding occurs, but the pregnancy may continue.
- Complete Miscarriage: The body expels all pregnancy tissue.
- Incomplete Miscarriage: Some tissue remains in the uterus.
- Missed Miscarriage: The embryo stops developing, but the body does not expel it.
- Recurrent Miscarriage: Three or more miscarriages happen in a row.
Here’s a quick reference table:
| Type of Miscarriage | Description |
|---|---|
| Threatened | Bleeding, but the pregnancy may still continue. |
| Complete | All pregnancy tissue is expelled. |
| Incomplete | Some tissue remains inside. |
| Missed | Embryo stops growing, but no bleeding occurs. |
| Recurrent | Three or more miscarriages in a row. |
Understanding these types can help you and your doctor make informed decisions. Each type may require different care and follow-up.
Common Causes
Many factors can lead to miscarriages. Some causes are more common than others. Here are several known causes:
- Chromosomal Abnormalities: Most miscarriages happen due to genetic issues.
- Uterine Abnormalities: Irregular shapes or fibroids can affect pregnancy.
- Hormonal Imbalances: Issues with hormones can disrupt pregnancy.
- Medical Conditions: Diabetes, thyroid issues, and autoimmune diseases are examples.
- Age: Women over 35 may face higher risks.
Here’s a summary of some common causes:
| Cause | Description |
|---|---|
| Chromosomal | Genetic problems in the embryo. |
| Uterine | Problems with the shape or structure of the uterus. |
| Hormonal | Imbalances in pregnancy-related hormones. |
| Medical Conditions | Chronic illnesses that affect health. |
| Age | Increased risk for women over 35. |
Understanding these causes can help you seek appropriate care. It also provides hope for future pregnancies.
Medical Evaluation
Many women wonder, “Can I get pregnant after three miscarriages?” This question often leads to a significant need for a medical evaluation. A thorough assessment helps identify potential issues. Understanding these factors can provide hope for future pregnancies. A medical evaluation can reveal underlying conditions affecting fertility and pregnancy.
Tests And Assessments
After experiencing three miscarriages, a series of tests and assessments can help clarify the situation. Doctors may recommend the following:
- Blood Tests: These check hormone levels and detect conditions like thyroid disorders.
- Genetic Testing: This helps identify potential genetic issues in parents.
- Ultrasound: This imaging test examines the uterus for abnormalities.
- Hysterosalpingography (HSG): This X-ray checks the fallopian tubes and uterus.
Here’s a simple table that summarizes these tests:
| Test Type | Purpose |
|---|---|
| Blood Tests | Check hormone levels and identify disorders |
| Genetic Testing | Identify genetic issues in parents |
| Ultrasound | Examine uterus for abnormalities |
| HSG | Check fallopian tubes and uterus |
These assessments provide valuable insights. They help doctors recommend effective treatment options. Understanding your body’s needs is crucial for a successful pregnancy.
Consulting A Specialist
Consulting a specialist is an important step after multiple miscarriages. A reproductive endocrinologist or a fertility specialist can offer expert advice. They specialize in diagnosing and treating fertility issues.
During your visit, the specialist will:
- Review your medical history.
- Discuss your miscarriage experiences.
- Conduct necessary tests.
- Provide tailored treatment options.
Seeking a specialist can help in several ways:
- Expert Guidance: Specialists understand complex fertility issues.
- Personalized Care: They create a plan that fits your needs.
- Emotional Support: Miscarriages can be emotionally taxing. Specialists provide support and resources.
Finding the right specialist can make a significant difference. They can help you navigate the path to a healthy pregnancy.

Credit: www.shecares.com
Fertility Factors
The journey to pregnancy can be challenging, especially after experiencing three miscarriages. Many women wonder about their fertility factors. Understanding these factors is crucial for anyone trying to conceive. Age and health play significant roles in fertility. Lifestyle choices also impact reproductive health. Both areas can influence the chances of getting pregnant again.
Age And Health
Age is a vital factor affecting fertility. As women age, their ability to conceive naturally decreases. The risk of miscarriage also rises. Here are some key points about age and health:
- Women in their 20s: Highest fertility rates.
- Women in their 30s: Fertility starts to decline.
- Women in their 40s: Significant drop in fertility.
Health conditions can also affect fertility. Conditions like polycystic ovary syndrome (PCOS) or thyroid issues can complicate getting pregnant. Regular check-ups help identify these conditions early.
| Age Range | Fertility Rate | Miscarriage Risk |
|---|---|---|
| 20-24 | High | 10% |
| 30-34 | Moderate | 15% |
| 35-39 | Lower | 20% |
| 40+ | Very Low | 50% |
Maintaining good health is essential. A balanced diet, regular exercise, and managing stress can improve fertility. Consult a healthcare provider for personalized advice.
Lifestyle Choices
Lifestyle choices significantly impact fertility. Factors such as diet, exercise, and habits can either enhance or hinder chances of conception. Here are some key aspects:
- Diet: A healthy diet supports reproductive health. Include fruits, vegetables, whole grains, and lean proteins.
- Exercise: Regular physical activity boosts overall health. Aim for at least 30 minutes of moderate exercise most days.
- Avoid harmful substances: Smoking, alcohol, and drugs can reduce fertility.
Stress management is equally important. High stress can disrupt hormones and affect ovulation. Consider relaxation techniques such as yoga or meditation.
Here’s a quick checklist of healthy lifestyle choices:
- Eat a balanced diet.
- Stay active.
- Manage stress levels.
- Avoid smoking and excessive alcohol.
- Regular medical check-ups.
Making positive lifestyle changes can improve your chances of a healthy pregnancy. Small adjustments in daily routines can yield significant benefits.
Next Steps After Miscarriage
Experiencing multiple miscarriages can be heartbreaking. It raises questions about future pregnancies. After three miscarriages, many wonder, “Can I get pregnant again?” Understanding the next steps after miscarriage is crucial. This journey involves emotional healing and physical readiness. Proper timing and a solid healing process are essential for future pregnancies.
Timing For Pregnancy
Choosing the right time for pregnancy after a miscarriage is vital. Each woman’s body is unique. The timing can affect both physical and emotional health. Here are some key points to consider:
- Physical Recovery: Wait for your body to heal. This may take a few weeks.
- Emotional Readiness: Take time to grieve. Emotional healing is important.
- Consult Your Doctor: Always seek medical advice before trying again.
Research shows that many doctors recommend waiting at least three months before trying to conceive again. This allows the uterus to recover fully. Here’s a simple table to summarize the recommended waiting times:
| Type of Miscarriage | Recommended Waiting Period |
|---|---|
| First Trimester Miscarriage | 1-3 months |
| Second Trimester Miscarriage | 3-6 months |
| Third Trimester Loss | 6-12 months |
Everyone’s situation differs. Listen to your body and seek professional advice. This approach helps ensure a healthier pregnancy next time.
Healing Process
Healing after a miscarriage is essential for future pregnancies. The process is both emotional and physical. It can take time to feel whole again. Here are steps to support your healing:
- Seek Support: Talk to friends, family, or a therapist. Sharing feelings helps.
- Practice Self-Care: Take time for yourself. Engage in relaxing activities.
- Stay Informed: Educate yourself about miscarriage and recovery. Knowledge empowers.
Creating a plan can guide your healing journey. Consider these activities:
- Join a support group.
- Keep a journal to express feelings.
- Engage in physical activities like yoga or walking.
Physical healing is also crucial. Your doctor can help you with this. Regular check-ups ensure your body is ready for pregnancy. Prioritize your emotional well-being. Healing takes time, but it prepares you for a healthy future pregnancy.
Support Systems
Experiencing three miscarriages can be emotionally challenging. Many women wonder about their future pregnancies and their support systems. Finding the right support can help navigate these feelings. Seeking help from professionals or connecting with others can make a significant difference. Understanding your options is vital for healing and planning ahead.
Counseling Options
Counseling can provide a safe space to express feelings. It helps in understanding grief and loss. Various counseling options are available:
- Individual Therapy: A therapist can guide you through personal feelings.
- Couples Counseling: This helps both partners cope and communicate better.
- Grief Counseling: Specializes in dealing with loss and emotional pain.
Many counselors use different techniques:
| Technique | Description |
|---|---|
| Cognitive Behavioral Therapy | Focuses on changing negative thought patterns. |
| Art Therapy | Uses creative expression to process emotions. |
| Supportive Counseling | Offers emotional support and understanding. |
Finding a qualified counselor is crucial. Look for someone experienced in pregnancy loss. Check reviews or get recommendations from friends or doctors.
Support Groups
Support groups can be invaluable. They connect people with shared experiences. Many find comfort in knowing they are not alone. Groups offer a chance to share stories and feelings.
- Online Support Groups: Join forums or social media groups.
- Local Meetups: Attend gatherings in your community.
- Specialized Organizations: Many offer resources and connections.
Support groups provide various benefits:
- Shared experiences can create bonds.
- Members can provide emotional support.
- Learning coping strategies from others can be helpful.
Many groups are led by professionals or trained volunteers. This ensures a safe and supportive environment. Look for groups that focus on pregnancy loss for the best fit.
Pregnancy Risks
Getting pregnant after three miscarriages can bring many worries. It’s normal to feel anxious about possible risks. Understanding these risks helps in planning for a healthy pregnancy. Some women may face complications. These can affect both the mother and the baby. Knowing what to expect can ease fears and provide hope.
Potential Complications
Pregnancy after multiple miscarriages may involve several complications. Each woman’s experience is unique. Here are some common issues that may arise:
- Recurrent Miscarriage: This means having multiple miscarriages in a row.
- Preterm Labor: This is when labor starts before 37 weeks.
- Low Birth Weight: Babies may be born smaller than normal.
- Gestational Diabetes: Some women may develop diabetes during pregnancy.
Here’s a table of potential complications:
| Complication | Description |
|---|---|
| Recurrent Miscarriage | Multiple pregnancies ending before 20 weeks. |
| Preterm Labor | Labor that begins before 37 weeks of pregnancy. |
| Low Birth Weight | Babies born weighing less than 5 pounds, 8 ounces. |
| Gestational Diabetes | High blood sugar levels during pregnancy. |
It’s essential to discuss these risks with a healthcare provider. They can offer guidance and support during this time.
Monitoring Pregnancy
Careful monitoring during pregnancy is crucial. Regular check-ups help ensure both mother and baby are healthy. Here are some ways to monitor a pregnancy:
- Frequent Ultrasounds: These help track the baby’s growth and development.
- Blood Tests: These check hormone levels and overall health.
- Regular Heartbeat Checks: Doctors monitor the baby’s heartbeat for any issues.
Consider these points for effective monitoring:
- Schedule regular appointments with your doctor.
- Follow your doctor’s advice on lifestyle changes.
- Communicate any concerns or symptoms immediately.
Staying informed and proactive helps in managing risks. A strong support system is also beneficial. Family and friends can provide emotional support during this journey.
Nutrition And Wellness
Many women wonder, “Can I get pregnant after 3 miscarriages?” This question often brings anxiety and uncertainty. Focusing on nutrition and wellness can help improve overall health. A balanced diet and proper supplements may support your body during this journey. Good nutrition can enhance fertility and create a healthier environment for pregnancy.
Dietary Changes
Making simple dietary changes can boost your chances of getting pregnant. A diet rich in whole foods can improve overall health. Here are some important food groups to include:
- Fruits and Vegetables: Aim for a rainbow of colors. These foods provide essential vitamins and antioxidants.
- Whole Grains: Choose brown rice, quinoa, and whole-wheat products. They are rich in fiber and nutrients.
- Lean Proteins: Include chicken, fish, beans, and nuts. These support healthy hormone levels.
- Dairy Products: Opt for low-fat milk, yogurt, and cheese. They are good sources of calcium and vitamin D.
Staying hydrated is vital. Drink plenty of water every day. Aim for at least 8 cups. Limit sugary drinks and caffeine. They can affect your fertility.
| Food Group | Benefits |
|---|---|
| Fruits & Vegetables | Rich in vitamins, minerals, and antioxidants |
| Whole Grains | Provide fiber and stabilize blood sugar |
| Lean Proteins | Support hormone balance and muscle health |
| Dairy Products | Provide calcium and support bone health |
Consider limiting processed foods and sugars. These can lead to inflammation and hormonal imbalances. A nutritious diet can create a healthy body ready for pregnancy.
Supplement Recommendations
Supplements can support your health and fertility. They fill gaps in your diet. Here are some recommended supplements:
- Folic Acid: Important for fetal development. Take at least 400 mcg daily.
- Vitamin D: Supports hormone function. Aim for 600 IU daily.
- Omega-3 Fatty Acids: Promote heart health and reduce inflammation. Look for 1000 mg daily.
- Iron: Supports blood health. Women should aim for 18 mg daily.
Always consult with a healthcare provider before starting any supplements. They can help determine the right dosages for your needs. Tracking your nutrition and supplement intake can help you stay on the right path.
| Supplement | Recommended Dosage | Benefits |
|---|---|---|
| Folic Acid | 400 mcg | Supports fetal development |
| Vitamin D | 600 IU | Enhances hormone function |
| Omega-3 Fatty Acids | 1000 mg | Reduces inflammation |
| Iron | 18 mg | Improves blood health |
Emotional Readiness
Having three miscarriages can deeply affect a woman’s emotional state. Many wonder, “Can I get pregnant after 3 miscarriages?” Before considering another pregnancy, emotional readiness is vital. It involves mental health, coping strategies, and support systems. Understanding these aspects helps in making informed decisions.
Mental Health Check
Emotional readiness starts with a mental health check. Miscarriages can lead to feelings of sadness, guilt, or anxiety. It’s essential to assess your emotional state before trying again. Here are some signs to consider:
- Persistent sadness that lasts weeks or months.
- Feelings of hopelessness or worthlessness.
- Increased anxiety about pregnancy or parenting.
- Difficulty concentrating or making decisions.
Consider seeking professional help if you notice these signs. A mental health professional can provide valuable support. Here’s a simple table to help you evaluate your mental health:
| Feeling | Frequency | Action |
|---|---|---|
| Sadness | Often | Talk to a therapist |
| Anxiety | Constantly | Practice relaxation techniques |
| Hopelessness | Sometimes | Reach out to friends |
Taking a mental health check is not just wise; it’s crucial. Understanding your feelings can help you prepare for future pregnancies.
Coping Mechanisms
Coping mechanisms can greatly enhance emotional readiness. After experiencing multiple miscarriages, finding effective ways to cope is essential. Here are some strategies:
- Talk about your feelings with friends or family.
- Join a support group for women who have faced similar experiences.
- Practice mindfulness to stay grounded and reduce anxiety.
- Engage in creative outlets such as writing or art.
Creating a support network is vital. Here’s how to build your support system:
- Identify trusted friends or family.
- Seek out online forums or local groups.
- Consider professional counseling for deeper support.
Utilizing these coping strategies can help you manage emotions effectively. They encourage healing and prepare you for the next steps in your journey.
Success Stories
Many women wonder, “Can I get pregnant after 3 miscarriages?” This question often comes with fear and uncertainty. Yet, countless women have shared their success stories. These stories inspire hope and show that it is possible to have a healthy pregnancy after multiple losses. Real-life experiences can provide comfort and strength to those on similar journeys.
Real-life Experiences
Many women have faced the heartache of miscarriage. Yet, many have gone on to have healthy pregnancies. Here are some inspiring stories:
- Emma’s Journey: After three miscarriages, Emma took a break. She focused on her health and well-being. After a year, she became pregnant again. Her baby girl is now a happy toddler.
- Sarah’s Story: Sarah had three losses in two years. She consulted a specialist who found a minor issue. After treatment, Sarah became pregnant again. She now has a beautiful baby boy.
- Linda’s Experience: After her third miscarriage, Linda joined a support group. Sharing her story helped her heal. With support, she tried again and welcomed twins into her family.
These stories show resilience. Many women faced challenges but found ways to overcome them.
Positive Outcomes
Success after multiple miscarriages is possible. Many women celebrate healthy pregnancies after their losses. Here are some key points about positive outcomes:
| Outcome | Details |
|---|---|
| Increased Support | Joining support groups can help share experiences. |
| Medical Guidance | Consulting specialists can identify underlying issues. |
| Emotional Healing | Many women find therapy beneficial for emotional health. |
Every journey is unique. Women often find strength through community and professional help. Listening to success stories can offer hope. It reminds many that dreams of motherhood can still come true.
Creating A Birth Plan
Experiencing three miscarriages can bring many emotions and questions. One common concern is the ability to get pregnant again. Creating a birth plan is essential for future pregnancies. A birth plan helps outline your wishes and preferences. It ensures that your healthcare team understands your needs. This plan can lead to a smoother pregnancy experience.
Involving Healthcare Providers
Involving your healthcare providers is crucial for a successful birth plan. They offer valuable insights and support. Discuss your experiences with them to build trust. A strong relationship with your providers makes it easier to share your concerns and wishes.
Here are some points to consider:
- Choose providers who respect your wishes.
- Ask questions about your past miscarriages.
- Seek guidance on any medical tests needed.
- Discuss potential risks in future pregnancies.
To help understand your options, consider this table:
| Provider Type | Role |
|---|---|
| Obstetrician | Manages pregnancy and delivery. |
| Midwife | Provides support during labor and birth. |
| Genetic Counselor | Offers advice on genetic risks. |
Having open conversations helps create a supportive environment. This way, you can focus on your journey to parenthood.
Preferences And Choices
Your preferences matter greatly in your birth plan. Knowing what you want can make a big difference. Think about your ideal birth experience. Do you prefer a hospital or home birth? Would you like a natural birth or pain relief options?
Consider these choices:
- Birth location: Home, hospital, or birthing center?
- Support persons: Who do you want with you?
- Pain relief: Natural methods or medication?
- Labor positions: Standing, sitting, or lying down?
Creating a list of preferences helps keep you focused. Share this list with your healthcare team. They can provide advice based on your choices. Here’s a simple way to organize your preferences:
- Write down your top three preferences.
- Discuss them with your provider.
- Adjust your plan as needed.
Your birth plan is about you. It reflects your hopes and desires. A well-prepared plan helps reduce stress and anxiety. This ensures a positive experience for you and your baby.

Credit: m.youtube.com
Importance Of Communication
After experiencing three miscarriages, many women wonder, “Can I get pregnant again?” This question brings a mix of emotions. Communication is vital during this time. It helps couples understand each other’s feelings and concerns. Open dialogue can ease anxiety and strengthen relationships. It also promotes a supportive environment for healing and planning for the future.
Talking With Partners
Talking openly with your partner is crucial after a loss. Sharing feelings can help both partners cope with grief. Here are some tips for effective communication:
- Choose the right time: Find a quiet moment to talk.
- Be honest: Share your feelings without holding back.
- Listen actively: Pay attention to your partner’s words.
- Validate emotions: Acknowledge each other’s pain and fears.
Both partners may experience different emotions. One might feel hopeful, while the other feels scared. It’s normal. Creating a safe space for discussions can help. You can consider having regular check-ins. This can be as simple as asking:
- How are you feeling today?
- What worries you the most?
- What are your hopes for the future?
Understanding each other’s feelings is key. It builds trust and closeness. A shared experience can strengthen your bond. Consider seeking professional help, like a therapist, if needed.
Engaging With Healthcare Team
Your healthcare team plays a crucial role in your journey. Open communication with them is essential. They can provide guidance and support tailored to your situation. Here’s how to engage effectively:
- Ask questions: Don’t hesitate to inquire about anything.
- Share your history: Tell them about your miscarriages.
- Discuss your goals: Explain your desire to conceive again.
Consider keeping a journal of your thoughts and questions. This can help you remember important topics. Here’s a simple table to organize your questions:
| Question | Notes |
|---|---|
| What tests should I consider? | To check for underlying issues. |
| How can I improve my chances? | Diet, exercise, and supplements. |
| What emotional support is available? | Therapists or support groups. |
Being open with your healthcare team helps them understand your needs. This can lead to better care and support. Remember, you are not alone in this journey.
Alternative Options
Experiencing three miscarriages can be heart-wrenching. Many wonder, “Can I get pregnant again?” While pregnancy may still be an option, some may seek alternative paths to parenthood. These alternatives can provide hope and fulfillment. Adoption and surrogacy are two popular options. Each has unique aspects to consider.
Adoption Considerations
Adopting a child can be a joyful choice. It opens doors to love and family. Here are some key points to think about:
- Types of Adoption:
- Domestic Adoption: Adopting within your country.
- International Adoption: Adopting from another country.
- Foster Care Adoption: Adopting children in the foster system.
- Adoption Process:
- Research adoption agencies.
- Complete an application.
- Attend training or workshops.
- Home study assessment.
- Match with a child.
- Finalize the adoption.
- Costs: Adoption can be expensive. Here’s a brief overview:
| Type of Adoption | Average Cost |
|---|---|
| Domestic Adoption | $20,000 – $40,000 |
| International Adoption | $30,000 – $50,000 |
| Foster Care Adoption | $0 – $2,500 |
Adoption can provide a loving home to a child in need. It can also offer a fulfilling experience for parents.
Surrogacy Possibilities
Surrogacy allows intended parents to have a biological connection to their child. This option involves a surrogate carrying the baby. Here are some key details:
- Types of Surrogacy:
- Traditional Surrogacy: The surrogate is the biological mother.
- Gestational Surrogacy: The surrogate carries an embryo created from the intended parents’ eggs and sperm.
- Surrogacy Process:
- Choose between traditional or gestational surrogacy.
- Find a surrogate through an agency or independently.
- Legal agreements are essential.
- Medical procedures to implant the embryo.
- Support during the pregnancy.
- Costs: Surrogacy can be costly. Here’s a breakdown:
| Type of Surrogacy | Average Cost |
|---|---|
| Traditional Surrogacy | $50,000 – $100,000 |
| Gestational Surrogacy | $100,000 – $150,000 |
Surrogacy can be a rewarding journey. It allows parents to experience the joy of having a child biologically related to them.
Future Family Planning
After experiencing three miscarriages, many women wonder about their chances of future pregnancies. Future family planning becomes a vital topic. Understanding timing and long-term health can help you make informed decisions. It’s essential to explore these aspects for better outcomes in the future.
Timing For Future Pregnancies
The timing of future pregnancies is crucial. Doctors often recommend waiting before trying again. This break allows the body to heal both physically and emotionally. Here are some factors to consider:
- Medical Advice: Always consult your healthcare provider.
- Emotional Readiness: Ensure you feel prepared mentally.
- Physical Recovery: Wait until your body is ready.
Many experts suggest waiting at least three months after a miscarriage. This waiting period can vary based on individual circumstances. Here’s a simple table to illustrate the suggested timing:
| Miscarriage Type | Recommended Waiting Time |
|---|---|
| Early Miscarriage | 1-3 months |
| Second Trimester Miscarriage | 3-6 months |
| Late Miscarriage | 6 months or more |
Each woman’s situation is different. Listen to your body and follow professional guidance. This careful approach can lead to a healthier pregnancy.
Long-term Considerations
Long-term considerations are essential for future family planning. After three miscarriages, it’s vital to assess overall health. Focus on both physical and emotional well-being.
- Regular Check-ups: Schedule regular visits with your doctor.
- Genetic Testing: Consider testing for potential genetic issues.
- Healthy Lifestyle: Maintain a balanced diet and exercise regularly.
Stress management is also important. Techniques like yoga and meditation can help. Support groups offer comfort and understanding. Here are some long-term strategies:
- Stay informed about your reproductive health.
- Communicate openly with your partner.
- Consider counseling to address emotional aspects.
Planning for the future requires patience and understanding. Each step taken helps build a stronger foundation for your family.
Resources And Support
Experiencing three miscarriages can be incredibly challenging. Many women wonder, “Can I get pregnant after three miscarriages?” Seeking the right resources and support is essential for healing. Knowledge helps build confidence and provides comfort during this time. Many organizations and materials can guide you through the emotional and physical journey of pregnancy after loss.
Helpful Websites
Numerous websites offer valuable information and support for those who have experienced multiple miscarriages. These sites can provide community, expert advice, and resources for your journey.
- March of Dimes: Focuses on maternal and infant health. Offers resources for miscarriage and pregnancy loss.
- Resolve: A national infertility association. Provides support for women facing reproductive challenges.
- Miscarriage Association: Offers resources specifically for miscarriage support and information.
- American Pregnancy Association: Provides comprehensive information on pregnancy, including loss and recovery.
These websites often feature:
- Support groups
- Expert articles
- Q&A sections
Connecting with others who understand your experience is vital. Many offer online forums where you can share stories and find comfort.
Books And Articles
Reading can be a powerful way to understand your feelings. Several books and articles discuss pregnancy after miscarriages. They provide insights, coping strategies, and support.
| Title | Author | Description |
|---|---|---|
| It Starts with the Egg | Rebecca Fett | A practical guide to improving egg health. |
| Miscarriage: Women’s Experiences and Needs | Dr. J. G. Evans | Explores women’s emotional experiences during miscarriage. |
| Taking Charge of Your Fertility | Toni Weschler | Comprehensive guide to understanding fertility. |
These resources help many women navigate their journeys. Reading stories from others can provide hope and understanding. Look for articles in magazines and online platforms that focus on reproductive health and emotional wellness.
Conclusion
Experiencing multiple miscarriages can be emotionally challenging. Many women do go on to have healthy pregnancies afterward. Seeking medical advice is crucial for understanding your unique situation. Support from loved ones and professionals can also help. Remember, hope remains, and every journey is different.
Stay informed and be kind to yourself.
Why Have I Had 5 Miscarriages?
Recurrent miscarriages can result from genetic abnormalities, hormonal imbalances, or underlying health conditions. It’s essential to consult a healthcare professional.
Experiencing multiple miscarriages is emotionally and physically challenging. Various factors, such as genetic issues, hormonal imbalances, or health conditions like thyroid disorders or diabetes, may contribute. Lifestyle factors, including smoking, excessive caffeine, or obesity, also play a role. Proper diagnosis and treatment from a healthcare provider are crucial.
They may recommend tests to identify specific causes and offer tailored treatments. Emotional support from loved ones or support groups can help navigate this difficult journey. Understanding potential causes and seeking appropriate medical advice is vital for managing and addressing recurrent miscarriages effectively.
Emotional Impact
Experiencing multiple miscarriages can be devastating. The emotional toll of having five miscarriages is immense. Feelings of grief, sadness, and even guilt can overwhelm you. Understanding the emotional impact is crucial to finding ways to cope and seek support.
Coping Mechanisms
Developing effective coping mechanisms is essential for healing. Here are some strategies:
- Journaling: Writing down your thoughts and emotions can be therapeutic. It helps you process your feelings.
- Therapy: Speaking to a professional therapist provides a safe space to express your emotions.
- Mindfulness: Practicing mindfulness and meditation can reduce stress and anxiety.
- Exercise: Physical activity releases endorphins, which improve your mood.
- Art: Engaging in creative activities like painting or music can be an emotional outlet.
Here is a table summarizing these coping mechanisms:
| Coping Mechanism | Description |
|---|---|
| Journaling | Writing down thoughts and emotions |
| Therapy | Speaking to a professional therapist |
| Mindfulness | Practicing mindfulness and meditation |
| Exercise | Engaging in physical activity |
| Art | Creative activities like painting or music |
Support Systems
Having a strong support system is crucial. It provides comfort and helps you navigate through grief. Here are key support systems to consider:
- Family and Friends: Loved ones offer emotional support and understanding. They can be a shoulder to cry on.
- Support Groups: Joining a miscarriage support group connects you with others who have similar experiences.
- Online Communities: Participating in online forums and groups can provide a sense of belonging and shared experiences.
- Healthcare Providers: Your doctor or counselor can offer guidance and support tailored to your needs.
- Religious or Spiritual Guidance: For some, faith can be a source of comfort during difficult times.
Remember, you are not alone. Support systems can help you heal and find hope.
Medical Causes
Experiencing multiple miscarriages can be heart-wrenching. Understanding the medical causes behind recurrent pregnancy loss is crucial. Identifying the reasons helps in planning future pregnancies and seeking appropriate treatment. Below, we explore some common medical causes of multiple miscarriages.
Chromosomal Abnormalities
Chromosomal abnormalities are a leading cause of recurrent miscarriages. These abnormalities occur when there are issues with the chromosomes in the embryo. These can be due to:
- Aneuploidy: This refers to an abnormal number of chromosomes. It often results from errors during cell division.
- Translocations: Parts of one chromosome may break off and attach to another. This can cause genetic imbalances.
Many chromosomal abnormalities are random and beyond control. In some cases, one or both parents might carry a balanced translocation. This does not affect their health but can lead to miscarriages. Genetic testing can help identify such issues.
| Type of Abnormality | Description |
|---|---|
| Aneuploidy | Abnormal number of chromosomes |
| Translocations | Chromosome segments attach to other chromosomes |
Doctors may recommend preimplantation genetic testing during IVF. This can help ensure only healthy embryos are implanted. Genetic counseling might also be beneficial for couples facing recurrent miscarriages.
Hormonal Imbalances
Hormonal imbalances can significantly impact pregnancy. Hormones play a vital role in maintaining a healthy pregnancy. Common hormonal issues include:
- Progesterone deficiency: Progesterone prepares the uterine lining for pregnancy. Low levels can prevent the embryo from implanting properly.
- Thyroid disorders: Both hyperthyroidism and hypothyroidism can affect pregnancy. They can lead to miscarriage if untreated.
Polycystic ovary syndrome (PCOS) is another common hormonal condition. Women with PCOS often have irregular menstrual cycles and higher risk of miscarriage.
Here’s a table summarizing common hormonal issues:
| Hormonal Issue | Impact on Pregnancy |
|---|---|
| Progesterone Deficiency | Prevents proper implantation |
| Thyroid Disorders | Increases miscarriage risk |
Addressing hormonal imbalances often involves medication. Your doctor might prescribe hormone supplements or thyroid medication. Regular monitoring of hormone levels is essential for a healthy pregnancy.
Genetic Factors
Experiencing multiple miscarriages can be heartbreaking and confusing. One common reason for recurrent pregnancy loss is genetic factors. These factors can influence the development and health of the pregnancy, leading to miscarriage. Understanding genetic factors can provide insights and potential solutions.
Inherited Conditions
Sometimes, inherited conditions from one or both parents can cause miscarriage. These conditions are passed down through generations and can affect the baby’s development. Inherited conditions can result from abnormal chromosomes, which may lead to genetic disorders.
Common inherited conditions include:
- Balanced Translocations: Parts of chromosomes swap places, but no genetic material is lost or gained. Parents may not show symptoms, but this can lead to miscarriage.
- Single Gene Disorders: Mutations in a single gene can cause conditions like cystic fibrosis or sickle cell anemia, potentially leading to miscarriage.
- Chromosomal Abnormalities: Extra or missing chromosomes, such as in Down syndrome, can result in miscarriage.
Doctors can identify these conditions through genetic testing. Knowing about these conditions helps in planning and managing future pregnancies. Genetic counseling can provide support and information.
Parental Genetics
Parental genetics play a crucial role in pregnancy. If either parent carries abnormal genes, it can affect the baby’s development. Genetic mutations and chromosomal abnormalities in parents can increase miscarriage risk.
Key genetic factors include:
- Maternal Age: Older women have a higher risk of chromosomal abnormalities in eggs.
- Paternal Age: Sperm quality declines with age, leading to genetic issues.
- Genetic Mutations: Mutations in parental genes can lead to miscarriage.
Genetic testing for both parents can reveal potential issues. This testing includes karyotyping to check chromosome structure and genetic screening for mutations. Early identification can help in managing risks.
Parental genetics and inherited conditions are key factors in recurrent miscarriages. Understanding these genetic factors can aid in finding solutions and support for future pregnancies.
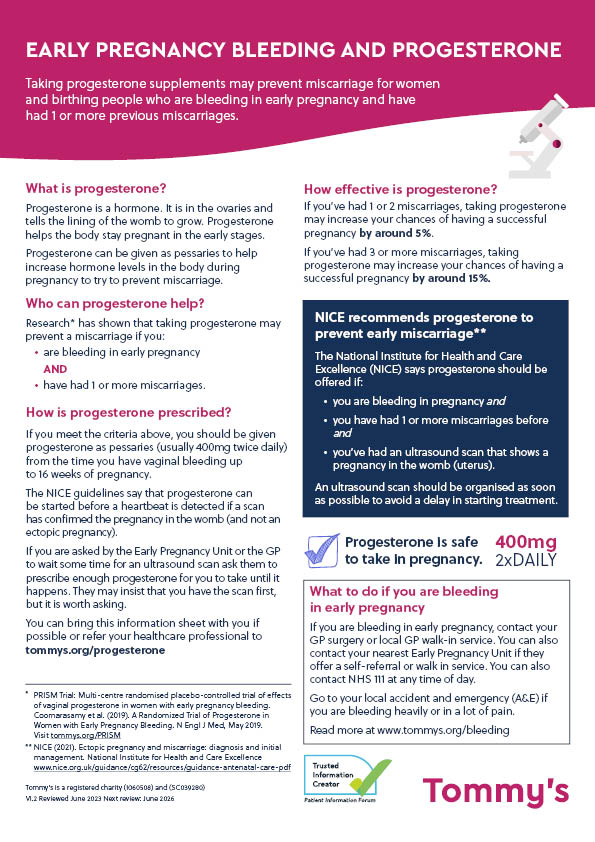
Credit: www.tommys.org
Lifestyle Choices
Experiencing multiple miscarriages can be heartbreaking. Understanding the reasons behind recurrent miscarriages is essential. One significant factor is lifestyle choices. Your daily habits, diet, and substance use can greatly impact your pregnancy. Let’s delve deeper into how these lifestyle choices might affect your ability to carry a pregnancy to term.
Diet And Nutrition
What you eat plays a vital role in your overall health and pregnancy. A balanced diet is crucial for a healthy pregnancy. Poor nutrition can lead to deficiencies that affect fetal development.
Consider the following dietary factors:
- Folic Acid: Essential for fetal development. Lack of folic acid increases the risk of neural tube defects.
- Iron: Prevents anemia. Anemia can cause complications during pregnancy.
- Calcium: Strengthens bones and teeth. Needed for the baby’s development.
- Protein: Building block of cells. Supports the baby’s growth.
- Hydration: Essential for maintaining amniotic fluid levels.
Here’s a simple table to show the daily recommended intake of these nutrients:
| Nutrient | Daily Recommended Intake |
|---|---|
| Folic Acid | 400-800 mcg |
| Iron | 27 mg |
| Calcium | 1000 mg |
| Protein | 71 grams |
| Water | 8-10 cups |
Avoid certain foods during pregnancy:
- Raw or undercooked meat
- Unpasteurized dairy products
- High-mercury fish
- Caffeinated drinks in large amounts
Substance Use
Substance use significantly affects pregnancy. Alcohol, tobacco, and drugs pose serious risks to both the mother and the fetus.
Alcohol consumption during pregnancy can lead to Fetal Alcohol Spectrum Disorders (FASD). Symptoms include physical abnormalities and cognitive deficits.
Tobacco smoking reduces oxygen supply to the fetus. It can cause low birth weight, preterm birth, and even stillbirth.
Drug use during pregnancy can lead to neonatal abstinence syndrome (NAS). Symptoms include tremors, irritability, and feeding difficulties.
Here’s a list of substances to avoid:
- Alcohol
- Tobacco
- Illegal drugs like cocaine, marijuana, and methamphetamine
- Some prescription medications (consult your doctor)
If you struggle with substance use, seek help. Speak with your healthcare provider. They can offer resources and support to ensure a healthier pregnancy.
Reproductive Health
Experiencing multiple miscarriages can be incredibly distressing. Understanding the underlying causes is crucial for addressing this issue. Reproductive health plays a significant role in the ability to carry a pregnancy to term. This section delves into various aspects of reproductive health that can impact pregnancy, particularly focusing on uterine abnormalities and cervical issues.
Uterine Abnormalities
Uterine abnormalities can significantly affect a woman’s ability to maintain a pregnancy. These abnormalities can be structural or functional. Here are some common uterine abnormalities:
- Septate Uterus: A septum or wall divides the uterus, leading to reduced space for the developing fetus.
- Bicornuate Uterus: The uterus has two cavities instead of one, which can cause complications.
- Fibroids: Noncancerous growths that can distort the uterine cavity, making it difficult for the embryo to implant properly.
- Asherman’s Syndrome: Scar tissue in the uterus, often from surgeries, can lead to miscarriages.
These issues can be diagnosed through imaging techniques such as:
| Technique | Description |
|---|---|
| Ultrasound | Uses sound waves to create images of the uterus. |
| Hysterosalpingography (HSG) | Involves injecting dye into the uterus and taking X-ray images. |
| Magnetic Resonance Imaging (MRI) | Provides detailed images using magnetic fields and radio waves. |
Treatments for uterine abnormalities may include surgical procedures to correct the structure or remove fibroids. Early diagnosis and treatment are essential for improving pregnancy outcomes.
Cervical Issues
Cervical issues can also lead to recurrent miscarriages. The cervix is the lower part of the uterus that opens into the vagina. Cervical problems can prevent a pregnancy from reaching full term. Common cervical issues include:
- Cervical Incompetence: The cervix opens too early during pregnancy, leading to miscarriage.
- Cervical Infections: Infections can cause inflammation and weaken the cervix.
- Previous Cervical Surgeries: Procedures like cone biopsy can weaken the cervix.
Diagnosing cervical issues may involve:
- Physical examinations.
- Ultrasound to measure cervical length.
- Testing for infections.
Treatment options for cervical issues might include:
- Cerclage: A surgical procedure where a stitch is placed to keep the cervix closed.
- Infection treatment: Antibiotics to clear any infections.
- Progesterone supplements: To strengthen the cervix.
Understanding and addressing cervical issues is crucial for reducing the risk of recurrent miscarriages. Regular prenatal care and early intervention can make a significant difference.

Credit: www.michellehartney.com
Age Considerations
Experiencing multiple miscarriages is heart-wrenching and often leads to many questions. One crucial factor to consider is age. Age plays a significant role in fertility and pregnancy outcomes. Understanding how age affects both maternal and paternal contributions can provide insights into recurrent miscarriages.
Maternal Age
Maternal age is a key factor in pregnancy success. As women age, the quality and quantity of their eggs decline. This decline begins in the early 30s and accelerates in the late 30s and 40s. By age 40, the chances of having a healthy pregnancy drop significantly.
Key points to understand about maternal age:
- Egg Quality: Older eggs have a higher risk of chromosomal abnormalities, leading to miscarriages.
- Hormonal Changes: Hormone levels fluctuate more with age, affecting ovulation and implantation.
- Health Conditions: Age increases the likelihood of conditions like hypertension and diabetes, which complicate pregnancy.
Here’s a table summarizing the risks associated with maternal age:
| Age Range | Miscarriage Rate |
|---|---|
| Under 30 | 10-15% |
| 30-34 | 15-20% |
| 35-39 | 20-25% |
| 40 and above | 40-50% |
Paternal Age
Paternal age also plays a role in pregnancy outcomes. Sperm quality declines as men age, although the impact is less dramatic than that of maternal age. Older paternal age can contribute to genetic abnormalities in the sperm, affecting embryo development and increasing the risk of miscarriage.
Key points to understand about paternal age:
- Sperm Quality: Sperm DNA fragmentation increases with age, leading to higher miscarriage rates.
- Genetic Mutations: Older sperm carry a higher risk of genetic mutations, which can cause developmental issues.
- Health Conditions: Older men are more likely to have health issues that affect sperm quality, such as obesity and chronic diseases.
Here’s a table summarizing the risks associated with paternal age:
| Age Range | Miscarriage Rate |
|---|---|
| Under 30 | 10-15% |
| 30-39 | 15-20% |
| 40-49 | 20-25% |
| 50 and above | 25-30% |
Understanding both maternal and paternal age considerations helps in addressing the potential causes of recurrent miscarriages. Discussing these factors with a healthcare provider can guide appropriate interventions and increase the chances of a successful pregnancy.
Environmental Factors
Experiencing multiple miscarriages can be heartbreaking. Understanding the causes is crucial. Environmental factors play a significant role in recurrent pregnancy loss. This section explores how toxins, chemicals, and workplace hazards can affect pregnancy.
Toxins And Chemicals
Exposure to toxins and chemicals can impact pregnancy. Harmful substances in everyday items might contribute to miscarriages. Some common sources of toxins include:
- Household cleaning products
- Personal care products
- Pesticides and herbicides
- Polluted air and water
Chemicals like BPA and phthalates are found in plastics. These can disrupt hormone levels. They might affect fetal development. Here is a table showing some common chemicals and their sources:
| Chemical | Source |
|---|---|
| BPA | Plastic containers, canned foods |
| Phthalates | Personal care products, plastics |
| Lead | Old paint, contaminated water |
| Mercury | Fish, industrial emissions |
Reducing exposure to these chemicals is essential. Use natural cleaning products. Choose BPA-free containers. Opt for organic foods. These small changes can make a big difference.
Workplace Hazards
Workplace hazards can also contribute to miscarriages. Women working in certain environments are at higher risk. Some hazardous workplaces include:
- Factories with chemical exposure
- Laboratories handling dangerous substances
- Healthcare settings with radiation
- Jobs requiring heavy lifting
Exposure to radiation and heavy metals can be harmful. They can affect both the mother and the fetus. Here is a list of common workplace hazards:
- Radiation from X-rays
- Chemical spills
- Biological hazards
- Heavy lifting
- Prolonged standing
Employers should ensure a safe working environment. They should provide protective gear. They should also limit exposure to harmful substances. Pregnant women should inform their employers about their pregnancy. This allows for necessary adjustments.
Understanding these environmental factors can help. Making informed choices can reduce the risk of miscarriage. Stay aware and take proactive steps for a healthier pregnancy.
Autoimmune Disorders
Experiencing multiple miscarriages can be incredibly heartbreaking. One possible cause for recurrent miscarriages is autoimmune disorders. These disorders cause the immune system to mistakenly attack the body’s own tissues. This can disrupt a pregnancy. Understanding the role of autoimmune disorders can help in managing and preventing miscarriages.
Lupus
Lupus is a chronic autoimmune disease. It causes inflammation in different parts of the body. This includes the skin, joints, and organs. For women with lupus, the risk of miscarriage is higher. This is due to the body’s immune system attacking healthy cells.
The most common symptoms of lupus include:
- Fatigue
- Joint pain
- Butterfly-shaped rash on the face
- Fever
Lupus can cause blood clots in the placenta. This disrupts the flow of nutrients to the baby. This can lead to miscarriage. Women with lupus should work closely with their doctors. They need to manage symptoms and monitor the pregnancy.
| Symptom | Effect on Pregnancy |
|---|---|
| Inflammation | Can cause placental problems |
| Blood Clots | Disrupts nutrient flow to the baby |
Regular check-ups and medications can help manage lupus during pregnancy. This reduces the risk of miscarriage.
Thyroid Issues
Thyroid issues are another common cause of miscarriage. The thyroid gland produces hormones that regulate metabolism. Both an overactive thyroid (hyperthyroidism) and an underactive thyroid (hypothyroidism) can affect pregnancy.
Common symptoms of thyroid issues include:
- Weight changes
- Fatigue
- Changes in heart rate
- Hair loss
Thyroid hormones play a crucial role in fetal development. Imbalances can lead to complications such as:
- Preterm birth
- Low birth weight
- Miscarriage
Women with thyroid issues should have their hormone levels monitored regularly. Medication can help manage these levels. This ensures a healthy pregnancy.
Regular monitoring and appropriate treatment are key. They help reduce the risk of miscarriage due to thyroid issues.
Infections
Experiencing multiple miscarriages can be heart-wrenching. One possible cause is infections. Infections can significantly impact pregnancy. Understanding the role of infections can help in addressing and potentially preventing further miscarriages.
Stis
Sexually Transmitted Infections (STIs) can affect pregnancy. They are infections passed from person to person through sexual contact. Several STIs can lead to miscarriages. These include:
- Chlamydia: This infection can cause inflammation in the reproductive organs. It can lead to complications in pregnancy.
- Gonorrhea: Gonorrhea can infect the uterus and fallopian tubes. This can result in ectopic pregnancy or miscarriage.
- Syphilis: Untreated syphilis can lead to severe pregnancy complications. This includes miscarriage, stillbirth, or premature birth.
- Herpes: Herpes infection during pregnancy can be harmful. It can cause miscarriage or premature labor.
It’s crucial to get tested for STIs if experiencing recurrent miscarriages. Early detection and treatment can make a significant difference. Safe sexual practices can also help in preventing these infections.
Other Infections
Besides STIs, other infections can also lead to miscarriages. Here are some common infections that can impact pregnancy:
- Bacterial Vaginosis: This is a bacterial infection in the vagina. It can increase the risk of preterm birth and miscarriage.
- Urinary Tract Infections (UTIs): UTIs can lead to complications if left untreated. They can cause kidney infections, which may result in miscarriage.
- Rubella (German Measles): Contracting rubella during pregnancy can be dangerous. It can lead to miscarriage or congenital defects.
- Listeria: This bacterial infection is often found in contaminated food. It can cause serious pregnancy complications, including miscarriage.
Regular prenatal check-ups can help detect and treat these infections early. Pregnant women should also avoid risky foods and maintain good hygiene to reduce the risk of infections.
Here’s a quick summary of these infections and their effects:
| Infection | Impact on Pregnancy |
|---|---|
| Chlamydia | Inflammation, complications |
| Gonorrhea | Ectopic pregnancy, miscarriage |
| Syphilis | Miscarriage, stillbirth |
| Herpes | Miscarriage, premature labor |
| Bacterial Vaginosis | Preterm birth, miscarriage |
| UTIs | Kidney infections, miscarriage |
| Rubella | Miscarriage, congenital defects |
| Listeria | Miscarriage, serious complications |
Addressing infections can be a key step in preventing further miscarriages. Discuss concerns with a healthcare provider for personalized advice and treatment.

Credit: www.reddit.com
Stress And Anxiety
Experiencing multiple miscarriages can be heart-wrenching. Many factors contribute to recurrent pregnancy loss, but stress and anxiety play significant roles. Understanding the link between mental health and physical effects can shed light on why miscarriages happen.
Mental Health
Stress and anxiety significantly impact mental health. They can disrupt the balance needed for a healthy pregnancy. Women experiencing high stress levels may face emotional turbulence, creating a challenging environment for conception and pregnancy maintenance.
Chronic stress leads to prolonged exposure to stress hormones like cortisol. Elevated cortisol levels can interfere with reproductive hormone regulation. This imbalance can make it harder for an embryo to implant or develop properly.
Anxiety disorders are also common among women with recurrent miscarriages. Anxiety can lead to:
- Sleep disturbances
- Appetite changes
- Constant worry
- Increased heart rate
These symptoms further strain the body, impacting overall health and well-being. Seeking support from mental health professionals can be beneficial. Therapy, mindfulness practices, and stress management techniques can help manage anxiety. Emotional support is crucial for navigating the challenges of recurrent pregnancy loss.
Physical Effects
Stress and anxiety don’t just affect mental health; they have profound physical effects. The body’s response to stress involves multiple systems, which can impact pregnancy viability.
Stress hormones like cortisol and adrenaline can affect blood flow to the uterus. Reduced blood flow can hinder the embryo’s ability to implant and grow. This physiological response to stress can increase the risk of miscarriage.
Immune system function can also be compromised under stress. A weakened immune system may struggle to protect the developing embryo. This vulnerability increases the likelihood of pregnancy complications.
High stress levels can lead to unhealthy behaviors such as:
- Poor diet
- Lack of exercise
- Substance use
These behaviors can further harm pregnancy outcomes. Maintaining a balanced lifestyle, including proper nutrition and regular physical activity, is vital. Reducing stress through relaxation techniques, yoga, and adequate rest can support a healthier pregnancy journey.
Previous Pregnancy History
Facing multiple miscarriages can be heartbreaking. Understanding your previous pregnancy history is essential to uncovering potential causes and finding solutions. Your past experiences can provide vital clues and help healthcare providers offer better support.
Past Losses
Evaluating your past pregnancy losses can reveal patterns that may explain recurrent miscarriages. Each loss is unique, but certain factors often stand out. These include:
- Timing of miscarriages: Were they early or later in pregnancy?
- Symptoms experienced: Cramping, bleeding, or no symptoms?
- Medical diagnosis: Any identified causes like genetic issues or uterine abnormalities?
By examining these aspects, doctors can determine if common factors exist. For example, if all losses occurred in the first trimester, this could indicate a genetic issue. A table summarizing your past losses might look like this:
| Pregnancy Number | Trimester | Symptoms | Diagnosis |
|---|---|---|---|
| 1 | First | Bleeding, Cramping | Unknown |
| 2 | Second | No Symptoms | Uterine Abnormality |
| 3 | First | Bleeding | Genetic Issue |
| 4 | First | Cramping | Unknown |
| 5 | First | Bleeding | Unknown |
Recording and analyzing this data can help pinpoint potential issues. This, in turn, allows for targeted tests and treatments that may prevent future losses.
Successful Pregnancies
Having experienced successful pregnancies can also provide valuable insights. These pregnancies can offer clues about what may have gone right. Reflecting on these experiences includes:
- Health during pregnancy: Were there specific lifestyle or health changes?
- Medical support: Did you receive any special treatments or medications?
- Stress levels: How did your emotional well-being impact the pregnancy?
For instance, maintaining a healthy diet and managing stress may have contributed to a successful pregnancy. Here’s a table summarizing successful pregnancies:
| Pregnancy Number | Trimester | Health Factors | Support Received |
|---|---|---|---|
| 1 | Full-term | Healthy Diet, Regular Exercise | Regular Check-ups, Prenatal Vitamins |
| 2 | Full-term | Stress Management, Healthy Diet | Specialist Consultations, Medications |
These insights can guide future pregnancies by replicating beneficial practices. The goal is to identify positive patterns that supported a healthy pregnancy and apply them to future attempts.
Medical Evaluations
Having multiple miscarriages can be heartbreaking. Understanding the reasons behind recurrent miscarriages is essential. Medical evaluations play a crucial role in identifying potential causes. They help guide treatment options and provide hope for future pregnancies.
Tests And Screenings
Doctors often recommend various tests and screenings to uncover underlying issues. Blood tests can reveal hormonal imbalances, clotting disorders, or genetic issues. Here are some common tests:
- Thyroid Function Tests: Check for thyroid hormone levels.
- Hormone Levels: Assess levels of progesterone and other hormones.
- Genetic Testing: Identify chromosomal abnormalities in parents or fetus.
Ultrasound scans are another essential tool. They help visualize the uterus and ovaries. Doctors look for structural abnormalities, like fibroids or polyps. Hysterosalpingography (HSG) is an X-ray procedure. It examines the shape of the uterus and fallopian tubes. Let’s explore these common tests in a table format:
| Test Name | Purpose |
|---|---|
| Thyroid Function Tests | Check thyroid hormone levels |
| Hormone Levels | Assess levels of progesterone and other hormones |
| Genetic Testing | Identify chromosomal abnormalities |
| Ultrasound Scans | Visualize uterus and ovaries |
| Hysterosalpingography (HSG) | Examine uterus and fallopian tubes |
Consultations
Consultations with specialists can provide deeper insights. Reproductive endocrinologists focus on hormonal and reproductive issues. They can recommend personalized treatment plans. Genetic counselors help understand genetic risks. They provide guidance on genetic testing results.
Psychological support is also vital. Counselors and therapists help manage emotional stress. Here are some essential consultations to consider:
- Reproductive Endocrinologist: Focus on reproductive health and hormonal issues.
- Genetic Counselor: Assist with understanding genetic testing and risks.
- Therapist: Provide emotional support and coping strategies.
Communication with healthcare providers is key. Ask questions and share concerns. Keep a record of all tests and results. This helps in tracking progress and making informed decisions.
Regular consultations ensure a comprehensive approach. They bring together medical, genetic, and emotional support. This holistic approach can improve the chances of a successful pregnancy.
Future Pregnancies
Facing multiple miscarriages can be deeply challenging and emotionally draining. Many wonder, “Why have I had 5 miscarriages?” Understanding the reasons and preparing for future pregnancies is essential. This section offers guidance on planning ahead and monitoring changes to increase the chances of a successful pregnancy.
Planning Ahead
After experiencing multiple miscarriages, planning ahead becomes crucial. Here are some steps to consider:
- Consult a Specialist: Seek help from a fertility specialist or a gynecologist. They can run necessary tests to identify potential issues.
- Genetic Testing: Both partners should consider genetic testing to rule out chromosomal abnormalities.
- Healthy Lifestyle: Adopting a healthy lifestyle can improve fertility. This includes a balanced diet, regular exercise, and avoiding alcohol and tobacco.
- Supplement Intake: Folic acid and prenatal vitamins are vital. They support fetal development and reduce the risk of certain defects.
- Medication Management: Discuss any medications you’re taking with your doctor. Some drugs may interfere with pregnancy.
Here’s a table summarizing key steps:
| Step | Description |
|---|---|
| Consult a Specialist | Seek expert advice to identify underlying issues. |
| Genetic Testing | Rule out chromosomal problems in both partners. |
| Healthy Lifestyle | Follow a balanced diet and regular exercise routine. |
| Supplement Intake | Take folic acid and prenatal vitamins as advised. |
| Medication Management | Review current medications with a healthcare provider. |
Monitoring Changes
Monitoring changes during pregnancy is vital for those with a history of miscarriages. Here are some key aspects to focus on:
- Regular Check-ups: Schedule frequent visits with your doctor. Regular monitoring ensures any issues are detected early.
- Ultrasounds: Ultrasounds help track the baby’s growth and development. They also check for any abnormalities.
- Blood Tests: Blood tests can monitor hormone levels, such as hCG and progesterone. These hormones are crucial for maintaining pregnancy.
- Lifestyle Adjustments: Maintain a stress-free environment. Stress can negatively impact pregnancy.
- Symptom Tracking: Keep a diary of any symptoms or changes. Share these with your doctor during visits.
Here’s a table summarizing monitoring steps:
| Step | Description |
|---|---|
| Regular Check-ups | Ensure frequent doctor visits to monitor progress. |
| Ultrasounds | Track baby’s growth and detect abnormalities. |
| Blood Tests | Monitor hormone levels crucial for pregnancy. |
| Lifestyle Adjustments | Reduce stress and create a supportive environment. |
| Symptom Tracking | Keep a record of symptoms to share with your doctor. |
Seeking Help
Experiencing multiple miscarriages can be an incredibly difficult and confusing time. If you’ve had five miscarriages, it’s essential to seek help to understand the underlying causes and find the support you need. This section focuses on the steps you can take to get the right help.
Specialist Referrals
After multiple miscarriages, getting a referral to a specialist is crucial. These experts can help identify any underlying medical issues. Start by consulting your primary care doctor or OB-GYN. They can refer you to reproductive endocrinologists or genetic counselors. Here are some key specialists you might encounter:
- Reproductive Endocrinologists: These doctors specialize in hormonal and reproductive health. They can run tests to check for hormonal imbalances, which can affect pregnancy.
- Genetic Counselors: These professionals assess genetic factors that might contribute to recurrent miscarriages. They can recommend genetic testing for you and your partner.
- Immunologists: These specialists focus on immune system issues that might cause miscarriages. They can test for autoimmune disorders or other immune-related problems.
Getting a specialist referral is a crucial first step. Here is a simple table to outline the types of tests each specialist might recommend:
| Specialist | Possible Tests |
|---|---|
| Reproductive Endocrinologist | Hormonal Tests, Ultrasound, Hysteroscopy |
| Genetic Counselor | Genetic Screening, Karyotyping |
| Immunologist | Autoimmune Tests, Blood Tests |
Support Groups
Emotional support is just as vital as medical help. Joining a support group can offer you a sense of community and understanding. These groups consist of people who have gone through similar experiences. They can provide emotional support and practical advice. Here are some benefits of joining support groups:
- Shared Experiences: Hearing others’ stories can help you feel less alone. It can be comforting to know you’re not the only one going through this.
- Emotional Relief: Talking about your feelings can be therapeutic. Support groups provide a safe space for you to express your emotions.
- Practical Advice: Members often share tips and resources. This can include recommendations for doctors, books, or coping strategies.
Consider both local and online support groups. Local groups offer face-to-face interaction, which can be very comforting. Online groups provide flexibility and can be accessed from the comfort of your home. Here are some popular support group options:
- Local Hospital Programs: Many hospitals offer support groups. Check with your healthcare provider for recommendations.
- Online Communities: Websites like BabyCenter or Reddit have active forums. These platforms are great for connecting with others.
- Non-Profit Organizations: Groups like Resolve or the Miscarriage Association offer both local and online support.
Joining a support group can make a big difference. It can help you feel more empowered and less isolated. Don’t hesitate to reach out and find the support you need.
Hope And Recovery
Experiencing multiple miscarriages can be heart-wrenching and confusing. Understanding the reasons behind recurrent miscarriages is crucial. Yet, amid the pain, hope and recovery are possible. This journey can lead to healing and renewed strength.
Finding Closure
Finding closure after multiple miscarriages is essential for emotional well-being. It’s a process that involves understanding, acceptance, and peace. Here are some steps to help:
- Seek Professional Help: Consulting a specialist can provide answers and a plan moving forward.
- Join Support Groups: Sharing experiences with others who understand can be comforting.
- Personal Reflection: Writing about your feelings in a journal can aid in processing emotions.
- Memorialize the Loss: Creating a small memorial or ritual can help honor the lost pregnancies.
It might also help to understand potential causes:
| Possible Cause | Description |
|---|---|
| Genetic Issues | Chromosomal abnormalities in the embryo. |
| Hormonal Imbalances | Problems like thyroid issues or PCOS. |
| Immune System Disorders | Conditions where the body attacks the embryo. |
| Structural Issues | Problems with the uterus or cervix. |
Understanding these factors can bring a sense of closure. It’s a step towards peace and acceptance.
Building Resilience
Building resilience is key in the journey towards hope and recovery. Resilience helps in coping with loss and moving forward. Here are some ways to build resilience:
- Practice Self-Care: Engage in activities that promote physical and mental well-being.
- Stay Connected: Keep in touch with loved ones and seek their support.
- Set Realistic Goals: Focus on small, achievable goals to regain a sense of control.
- Learn Stress Management Techniques: Techniques like meditation and yoga can be very helpful.
Another important aspect is finding strength in your story:
- Share Your Experience: Talking about your journey can be empowering and healing.
- Focus on Positives: Look for silver linings and celebrate small victories.
- Seek Professional Guidance: Therapy can provide tools to manage grief and build resilience.
Remember, resilience is not about forgetting the loss. It’s about learning to live with it and finding joy in life again. Each step taken towards resilience is a step towards healing.
Conclusion
Understanding the reasons behind multiple miscarriages is crucial. Consult with healthcare professionals for personalized advice. Each case is unique, so professional guidance is essential. Prioritize your health and well-being. Seek support from loved ones and support groups. You’re not alone on this journey.
What Week is the Highest Risk of Miscarriage?
The highest risk of miscarriage occurs during the first 12 weeks of pregnancy. Most miscarriages happen in the first trimester.
Miscarriage is a common concern for many expecting parents. Understanding the critical periods can help in managing stress and seeking timely medical advice. The first trimester, which spans from week 1 to week 12, is when most miscarriages occur. During this stage, the embryo undergoes significant development, making it a vulnerable period.
Various factors, including genetic abnormalities, hormonal imbalances, and lifestyle choices, can contribute to the risk. Knowing this can encourage pregnant individuals to take necessary precautions and maintain regular prenatal check-ups. Early medical intervention and a healthy lifestyle can significantly improve pregnancy outcomes.

Credit: www.accessfertility.com
Key Miscarriage Statistics
Miscarriage is a deeply sensitive topic for many. Understanding the statistics can help expectant parents be better prepared. The highest risk of miscarriage is usually in the early weeks of pregnancy. Key miscarriage statistics provide insights into general rates and age-related factors.
General Rates
Miscarriage occurs in about 10-20% of known pregnancies. Most miscarriages happen in the first trimester. Some key points about general miscarriage rates include:
- About 80% of miscarriages occur within the first 12 weeks.
- The risk of miscarriage decreases significantly after the first trimester.
- Pregnancies that make it past the 20-week mark have a much lower risk.
A table summarizing the general rates:
| Pregnancy Stage | Miscarriage Risk |
|---|---|
| First Trimester (0-12 weeks) | 80% |
| Second Trimester (13-26 weeks) | 1-5% |
| Third Trimester (27-40 weeks) | <1% |
Age Factors
Age plays a significant role in miscarriage risk. Women over the age of 35 have a higher risk. Some key points regarding age factors:
- Women under 35 have a 15% risk of miscarriage.
- Women aged 35-45 have a 20-35% risk.
- Women over 45 have a 50% risk.
Here’s a detailed table showing miscarriage risk by age:
| Maternal Age | Miscarriage Risk |
|---|---|
| Under 35 | 15% |
| 35-40 | 20-25% |
| 40-45 | 35-45% |
| Over 45 | 50% |
Understanding these age factors helps in planning and preparing for a healthy pregnancy.

Credit: www.momjunction.com
First Trimester Risks
The first trimester is a critical period in pregnancy. Many women wonder about the highest risk of miscarriage during this time. Understanding first trimester risks can help expectant mothers take precautions. Knowing what to expect can reduce anxiety and provide peace of mind.
Weeks 1-4
The first four weeks of pregnancy are crucial. Most women don’t even know they’re pregnant during this stage. The fertilized egg travels to the uterus and implants itself. During this time, several factors can lead to miscarriage:
- Chromosomal abnormalities: The most common cause.
- Hormonal imbalances: Can prevent the egg from implanting properly.
- Health conditions: Like diabetes or thyroid issues.
- Lifestyle factors: Smoking, alcohol, and drug use.
Symptoms of miscarriage in weeks 1-4 may include:
- Heavy bleeding
- Severe cramping
- Passage of tissue
If any of these symptoms occur, contact a healthcare provider immediately. Early detection can sometimes prevent a miscarriage.
Weeks 5-7
Weeks 5 to 7 mark a significant phase. The embryo starts to develop major organs. Miscarriage risk remains high during this time. Causes of miscarriage during these weeks include:
- Genetic issues: Continue to be a primary cause.
- Infections: Like rubella or cytomegalovirus.
- Autoimmune disorders: Such as lupus.
- Physical trauma: Accidents or injuries.
Signs of a miscarriage in weeks 5-7 might include:
- Vaginal bleeding
- Abdominal pain
- Loss of pregnancy symptoms
A table summarizing risks and signs in weeks 5-7:
| Risks | Signs |
|---|---|
| Genetic issues | Vaginal bleeding |
| Infections | Abdominal pain |
| Autoimmune disorders | Loss of pregnancy symptoms |
Consult a doctor if you notice any concerning symptoms. Early intervention can be crucial in these weeks.
Peak Risk Week
Understanding the risk of miscarriage is crucial for expecting parents. Miscarriage can happen at different stages of pregnancy, but there is a specific period known as the Peak Risk Week. During this week, the chances of miscarriage are the highest, making it an important time for monitoring and care.
Week 6 Insights
Week 6 marks a critical stage in pregnancy. During this period, the embryo undergoes significant development. The heart starts beating, and major organs begin to form. Unfortunately, this is also the time when many miscarriages occur. Studies show that the risk of miscarriage peaks around Week 6.
Some key insights about Week 6 include:
- The embryo measures about 2-4mm in length.
- Signs of pregnancy like nausea and fatigue become more noticeable.
- Spotting or light bleeding can be common but should be monitored.
In Week 6, about 15-20% of known pregnancies end in miscarriage. This statistic underscores the need for careful observation and prompt medical attention during this stage. Seeking regular prenatal care can help in detecting any potential issues early.
| Developmental Milestone | Details |
|---|---|
| Heartbeat | Begins to beat |
| Length | 2-4 mm |
| Symptoms | Nausea, fatigue, spotting |
Factors Influencing Risk
Several factors influence the risk of miscarriage during the peak week. These factors can vary from genetic issues to lifestyle choices. Understanding these factors can help in mitigating risks.
Some key factors include:
- Genetic abnormalities: Chromosomal issues can prevent the embryo from developing properly.
- Hormonal imbalances: Low levels of progesterone can lead to miscarriage.
- Age of the mother: Women over 35 have a higher risk.
- Lifestyle choices: Smoking, alcohol consumption, and drug use increase the risk.
- Medical conditions: Conditions like diabetes and thyroid problems can affect pregnancy.
Let’s look at some statistics:
| Factor | Impact on Risk |
|---|---|
| Genetic Abnormalities | 50-70% of miscarriages |
| Maternal Age > 35 | 20-35% increased risk |
| Smoking | 1.5-2 times higher risk |
Awareness of these factors can help in taking preventive measures. Regular check-ups, a healthy lifestyle, and timely medical advice can significantly lower the risk of miscarriage during the peak risk week.
Signs Of Miscarriage
The highest risk of miscarriage typically occurs in the first trimester, specifically between weeks 6 and 12. Knowing the signs of miscarriage can help you seek medical attention promptly. Early detection is crucial for your health and well-being.
Physical Symptoms
Recognizing physical symptoms of miscarriage is essential. These symptoms may vary, but common signs include:
- Vaginal bleeding: This can range from light spotting to heavy bleeding. It may contain clots.
- Abdominal pain: Cramping in the lower abdomen, often resembling period cramps.
- Back pain: Persistent or severe pain in the lower back.
- Tissue passing: Passing tissue or clots from the vagina.
- Loss of pregnancy symptoms: Sudden disappearance of pregnancy symptoms like nausea and breast tenderness.
If you experience any of these symptoms, contact your healthcare provider immediately. They may perform an ultrasound or blood tests to confirm the status of your pregnancy.
| Symptom | Description |
|---|---|
| Vaginal Bleeding | Light spotting to heavy bleeding with clots |
| Abdominal Pain | Cramping in lower abdomen |
| Back Pain | Persistent or severe pain in the lower back |
| Tissue Passing | Passing tissue or clots from the vagina |
| Loss of Pregnancy Symptoms | Sudden disappearance of symptoms like nausea and breast tenderness |
Emotional Impact
Miscarriage affects not only the body but also the mind. The emotional impact can be profound.
Grief and sadness are common feelings. Many women feel a deep sense of loss. They mourn the future they imagined.
Guilt and self-blame may also arise. Some women wonder if they did something wrong. It’s important to understand that most miscarriages occur due to genetic factors beyond one’s control.
Anxiety and fear about future pregnancies can develop. Women may worry about the possibility of another miscarriage. Speaking with a counselor can help manage these fears.
- Grief and sadness: Feeling a deep sense of loss.
- Guilt and self-blame: Wondering if they did something wrong.
- Anxiety and fear: Concerns about future pregnancies.
Emotional support is crucial. Family, friends, and support groups can provide comfort and understanding. Seeking professional counseling can also be beneficial during this time.
Preventative Measures
Understanding the highest risk weeks of miscarriage is crucial for expecting parents. The highest risk typically occurs in the first trimester, especially between weeks 6 to 12. Knowing this, it’s important to take preventative measures to ensure a healthy pregnancy. These measures can significantly reduce the risk and support a safer journey to parenthood.
Healthy Lifestyle
Maintaining a healthy lifestyle is crucial during pregnancy. Here are some key practices:
- Balanced Diet: Ensure you eat a variety of fruits, vegetables, lean proteins, and whole grains.
- Avoid Harmful Substances: Stay away from alcohol, cigarettes, and drugs.
- Regular Exercise: Engage in moderate activities like walking or prenatal yoga.
- Stay Hydrated: Drink plenty of water throughout the day.
- Get Enough Sleep: Aim for at least 7-8 hours of quality sleep every night.
A balanced diet is critical. Here’s a simple table to guide your daily intake:
| Nutrient | Daily Requirement | Sources |
|---|---|---|
| Folic Acid | 400-800 mcg | Leafy greens, citrus fruits, beans |
| Calcium | 1000 mg | Dairy products, fortified cereals, leafy greens |
| Iron | 27 mg | Lean meat, spinach, legumes |
By following these guidelines, you can promote a healthy pregnancy and reduce the risk of miscarriage.
Medical Guidance
Regular medical guidance is essential during pregnancy. Make sure to:
- Schedule Prenatal Visits: Regular check-ups help monitor the baby’s health and development.
- Follow Medical Advice: Adhere to any recommendations from your healthcare provider.
- Take Prescribed Supplements: Prenatal vitamins, especially those containing folic acid, are important.
- Inform About Symptoms: Report any unusual symptoms like severe cramps, bleeding, or dizziness.
- Understand Medical History: Discuss any past medical issues or family history with your doctor.
Having a clear communication channel with your healthcare provider ensures timely interventions. This proactive approach greatly minimizes the risk of complications. Remember, consistent medical guidance significantly enhances the chances of a healthy pregnancy.
Credit: www.researchgate.net
Role Of Genetics
Miscarriage is a common concern for expectant mothers. Understanding the highest risk week for miscarriage helps in taking preventive measures. The role of genetics plays a significant part in miscarriage risks, especially during the early weeks of pregnancy. Genetic factors can affect the development of the fetus, leading to a higher chance of miscarriage.
Chromosomal Abnormalities
Chromosomal abnormalities are a major cause of miscarriage, particularly in the first trimester. These abnormalities occur when there is an error in the number or structure of chromosomes. This can hinder the normal development of the fetus.
Common types of chromosomal abnormalities include:
- Trisomy: An extra chromosome is present, like in Down syndrome.
- Monosomy: A missing chromosome, such as Turner syndrome.
- Translocation: Parts of chromosomes are rearranged.
Statistics show that around 50% of miscarriages in the first trimester are due to chromosomal abnormalities. This risk is highest between weeks 6 to 10. During this time, the embryo undergoes rapid cell division and growth. Any genetic errors during this critical period can lead to miscarriage.
| Type of Abnormality | Risk Factor |
|---|---|
| Trisomy | Extra Chromosome |
| Monosomy | Missing Chromosome |
| Translocation | Rearranged Chromosomes |
Family History
Family history also plays a crucial role in the risk of miscarriage. If there is a history of miscarriages in the family, the risk can be higher. This is due to inherited genetic mutations or conditions that can be passed down through generations.
Factors influenced by family history include:
- Inherited genetic mutations: Conditions like balanced translocations.
- Chronic health conditions: Diseases such as diabetes or thyroid disorders.
Studies indicate that women with a family history of miscarriages have a higher risk, especially during the first 12 weeks of pregnancy. It’s important to inform healthcare providers about any family history of miscarriages. This helps in monitoring and managing the pregnancy more effectively.
Genetic counseling can be beneficial for those with a family history of miscarriages. It provides insights into potential risks and preventive measures. Understanding the genetic factors involved helps in taking proactive steps to ensure a healthy pregnancy.
Support Systems
Experiencing a miscarriage can be a difficult and emotional time. The highest risk of miscarriage is typically during the first trimester, especially between weeks 6 and 12. During this period, a strong support system is crucial. Support systems provide emotional and practical assistance to those affected. They help you navigate through this challenging phase.
Counseling Options
Counseling is a vital support system for those coping with miscarriage. It offers a safe space to express feelings and get professional guidance. Counseling services can be accessed through:
- Hospitals and Clinics: Most hospitals have in-house counselors who specialize in grief and pregnancy loss.
- Private Therapists: Many therapists focus on reproductive health and can provide tailored support.
- Online Counseling: Platforms like BetterHelp and Talkspace offer virtual counseling sessions, making it easier to seek help from home.
Group therapy is another effective form of counseling. It connects you with others who have experienced similar losses. This shared understanding can be very comforting. Some benefits of group therapy include:
- Feeling less isolated.
- Learning coping strategies from others.
- Building a support network.
Consider these options and choose what feels right for you. A supportive counselor or group can make a significant difference during this time.
Community Resources
Community resources offer additional layers of support during a miscarriage. They often provide both emotional and practical help. Key community resources include:
- Support Groups: Many communities have local support groups that meet regularly. These groups offer a space to share experiences and gain support.
- Non-Profit Organizations: Organizations like The Miscarriage Association provide valuable information and support services. They often offer helplines, online forums, and resource materials.
- Faith-Based Organizations: Many religious groups offer counseling and support for those experiencing loss. Their services can include prayer groups, counseling, and community support.
- Local Health Departments: These departments can connect you with nearby resources and support services.
Online forums and communities are also excellent resources. Websites like Reddit and BabyCenter have forums where you can discuss your feelings anonymously and get advice from others. Benefits of online communities include:
| Benefit | Description |
|---|---|
| 24/7 Access | Support available any time of day. |
| Anonymity | Share your story without revealing your identity. |
| Wide Reach | Connect with people from all over the world. |
Engaging with community resources can provide a sense of belonging and support. These resources can help you feel less alone during this tough time.
After A Miscarriage
Miscarriage is a challenging and emotional experience for many. Knowing the highest risk weeks can help expectant parents prepare. Understanding the aftermath is also crucial. After a miscarriage, both emotional and physical healing are essential. Support systems and coping strategies play a vital role in recovery.
Coping Strategies
After a miscarriage, emotions can be overwhelming. Finding ways to cope is important for mental health. Here are some strategies that may help:
- Seek Support: Talking to friends, family, or a therapist can provide comfort.
- Join Support Groups: Sharing experiences with others who have gone through the same can be healing.
- Allow Yourself to Grieve: It’s natural to feel a range of emotions. Give yourself time to process them.
- Engage in Self-Care: Activities like reading, walking, or meditating can offer relaxation and peace.
Understanding your body’s healing process is also crucial. Here’s a table summarizing the physical recovery timeline:
| Time Frame | What to Expect |
|---|---|
| First Week | Bleeding and cramping are common. |
| Two to Four Weeks | Physical symptoms usually subside. |
| Six Weeks | Most women feel physically recovered. |
Remember, everyone heals at their own pace. Respect your journey and seek help if needed.
Future Pregnancies
Thinking about future pregnancies can bring both hope and fear. After a miscarriage, many wonder about their chances of conceiving again. Here are some key points to consider:
- Consult Your Doctor: A healthcare provider can offer guidance on when to try again.
- Understand Risks: Most women can have healthy pregnancies after a miscarriage. Recurrent miscarriages are rare.
- Monitor Your Health: Keeping a healthy lifestyle improves your chances. Eat well, exercise, and avoid stress.
- Track Your Cycle: Knowing your ovulation can help you plan better.
Emotional readiness is as important as physical health. Here are some signs you might be ready:
- You feel emotionally stable.
- You have discussed your feelings with your partner.
- Your doctor has given you the green light.
Future pregnancies can be filled with hope and joy. Every journey is unique. Stay positive and take one step at a time.
Conclusion
Understanding the highest risk weeks for miscarriage empowers you with knowledge. Early pregnancy requires extra care and attention. Regular check-ups and a healthy lifestyle can make a difference. Always consult with your healthcare provider for personalized advice. Your journey is unique, and support is available every step of the way.