Small Intestinal Bacterial Overgrowth, commonly abbreviated as SIBO, is a complex and often misunderstood condition affecting the small intestine, the crucial gut segment where most nutrient absorption occurs. This condition arises when there is an abnormal increase in the overall bacterial population in the small intestine, particularly types of bacteria not typically found in that part of the digestive system. Understanding SIBO is essential not only for those directly affected by the condition but also for healthcare professionals striving to provide optimal digestive health care.
Small Intestinal Bacterial Overgrowth (SIBO)
I. Understanding SIBO: Basics and Background
- Definition and Overview
- Explanation of SIBO
- Key functions of the small intestine in digestion and nutrient absorption
- Causes of SIBO
- Common physiological causes: motility issues, anatomical abnormalities, and pH changes
- Risk factors, including surgeries, diabetes, and chronic conditions affecting the gut
- Symptoms of SIBO
- Typical symptoms: bloating, pain, malabsorption, and malnutrition
- Systemic effects of SIBO: how excessive bacteria can impact overall health
II. Diagnosis and Challenges
- Diagnostic Techniques
- Breath tests: methodology and interpretation
- Use of jejunal aspirate culture
- Recent advances in diagnostic technologies
- Challenges in Diagnosing SIBO
- Overlap with symptoms of other digestive diseases like IBS
- Limitations of current diagnostic methods
III. Treatment Strategies
- Antibiotic Therapy
- First-line antibiotics for SIBO and their mechanisms
- Challenges with antibiotic resistance and recurrence
- Dietary Management
- Role of diet in managing SIBO
- Effective dietary strategies: Low FODMAP, gluten-free, and others
- Alternative Treatments
- Probiotics and their controversial role in SIBO treatment
- Herbal therapies and their efficacy
IV. Living with SIBO
- Daily Management
- Lifestyle changes to manage symptoms
- Importance of a tailored diet and regular follow-up
- Long-term Outlook
- Potential complications if left untreated
- Prognosis with proper treatment
V. Future Directions
- Research Trends
- Latest research on pathophysiology and treatment
- Innovations in gut microbiome management
- The Role of Technology
- How new technologies are shaping the future of SIBO diagnosis and treatment
VI. Conclusion
- Summary of key points
- The importance of awareness and education on SIBO
- Encouragement for ongoing research and improved management strategies
Small Intestinal Bacterial Overgrowth: A Detailed Overview
Small Intestinal Bacterial Overgrowth (SIBO) is a condition that affects the small intestine, leading to the growth of excessive bacteria that can interfere with normal digestion and absorption of nutrients. In this article, we will explore the various aspects of SIBO, including its definition, causes, symptoms, diagnosis, and treatment options, as well as the lifestyle modifications necessary to manage the condition. We will also dive into the latest research trends and advancements in SIBO diagnosis and treatment.
I. Understanding SIBO: Basics and Background
Definition and Overview
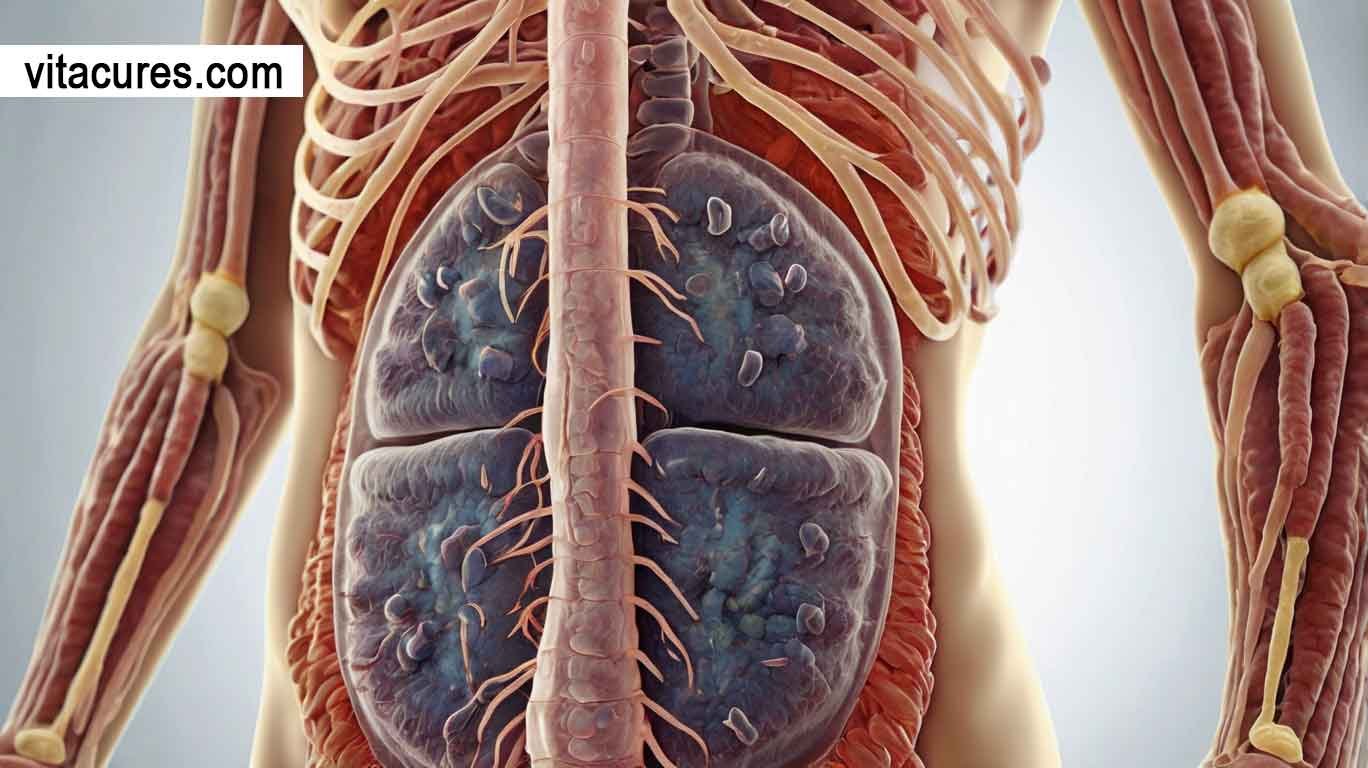
Small Intestinal Bacterial Overgrowth (SIBO) is a condition characterized by an abnormal increase in the number of bacteria in the small intestine. The small intestine is typically home to a relatively small population of bacteria compared to the colon. However, in SIBO, these bacteria proliferate and can lead to various digestive symptoms and malabsorption issues. Normally, the small intestine serves to digest food and absorb nutrients; however, when bacteria overgrow, they can interfere with this process, leading to discomfort and nutritional deficiencies.
Key Functions of the Small Intestine in Digestion and Nutrient Absorption
The small intestine plays a critical role in digestion by breaking down food into its basic components so that nutrients can be absorbed into the bloodstream. It is responsible for absorbing:
- Carbohydrates: broken down into sugars like glucose.
- Proteins: broken down into amino acids.
- Fats: broken down into fatty acids and glycerol.
- Vitamins and Minerals: Absorbed directly into the bloodstream.
When bacteria grow in the small intestine, they can consume nutrients before the body has a chance to absorb them, leading to malnutrition and a variety of gastrointestinal symptoms.
II. Causes of SIBO
Common Physiological Causes
SIBO can develop as a result of various physiological factors that disrupt the normal function of the small intestine. Some of the primary causes include:
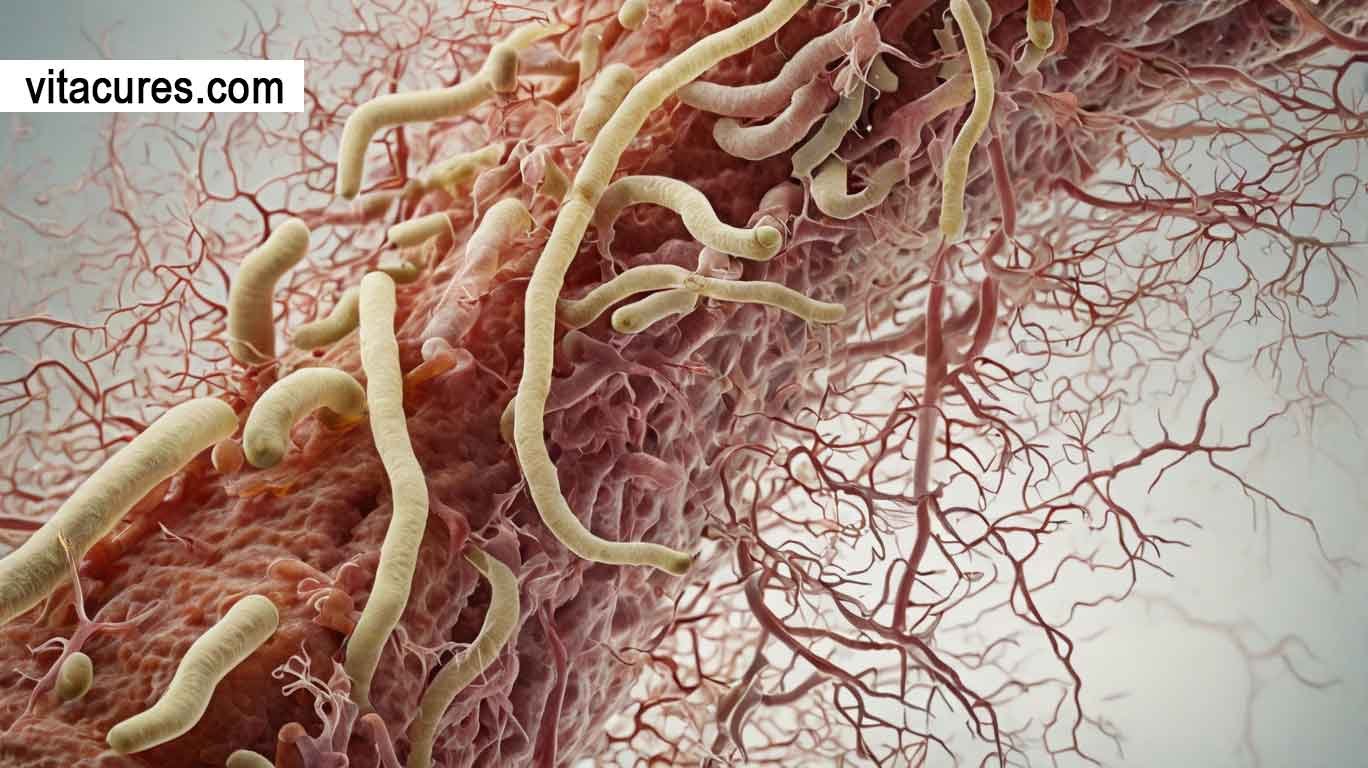
- Motility Issues:
- The small intestine relies on coordinated muscle contractions (peristalsis) to move food and waste through the digestive tract. When motility is impaired, such as in conditions like gastroparesis (delayed stomach emptying) or scleroderma (a connective tissue disorder), food and bacteria can stagnate, providing an environment conducive to bacterial overgrowth.
- Anatomical Abnormalities:
- Structural issues like intestinal diverticula (small pouches in the wall of the intestine), strictures, or surgical alterations (such as after gastric bypass surgery) can create pockets where bacteria can accumulate and multiply.
- pH Changes:
- The small intestine is normally slightly alkaline. If the stomach acid is reduced (for example, through the use of proton pump inhibitors or antacids), bacteria from the colon or mouth can thrive in the small intestine.
Risk Factors Including Surgeries, Diabetes, and Chronic Conditions Affecting the Gut
Certain conditions can increase the risk of developing SIBO:
- Surgical History: Previous surgeries that affect the gut, such as gastrectomy or bariatric surgery, can lead to anatomical changes that promote bacterial growth.
- Diabetes: High blood sugar levels can alter gut motility and the immune response, leading to an increased risk of SIBO.
- Chronic Conditions: Diseases like Celiac Disease, Crohn’s Disease, and IBS (Irritable Bowel Syndrome) can disrupt the normal balance of bacteria in the gut, making the small intestine more susceptible to bacterial overgrowth.
III. Symptoms of SIBO
SIBO can manifest in a variety of symptoms that overlap with other gastrointestinal conditions, which often makes diagnosis challenging. Common symptoms include:
- Bloating: Excess gas produced by bacteria fermenting undigested food can lead to bloating and discomfort.
- Pain or discomfort: This can include cramping, a feeling of fullness, or general abdominal pain.
- Malabsorption: Due to the overgrowth of bacteria in the small intestine, your body may struggle to absorb essential nutrients, leading to symptoms such as weight loss and deficiencies in vitamins (like B12 or fat-soluble vitamins).
- Nutritional Deficiencies: Individuals with SIBO may develop deficiencies in important nutrients like vitamin B12, iron, and calcium, potentially leading to fatigue, anemia, and weakened bone health.
Systemic Effects of SIBO
The impact of SIBO extends beyond the digestive system. The overgrowth of bacteria can affect the entire body, leading to:
- Fatigue due to nutrient malabsorption.
- Headaches are linked to vitamin deficiencies.
- Joint pain due to the inflammatory response triggered by bacterial overgrowth.
- Mental fog or brain fog due to nutritional deficiencies and chronic discomfort.
IV. Diagnosis and Challenges
Diagnostic Techniques
Accurate diagnosis of SIBO is crucial for effective treatment. There are several diagnostic approaches:
- Breath Tests:
- The lactulose breath test and glucose breath test are non-invasive methods used to detect SIBO. These tests measure hydrogen and methane levels in the breath after the ingestion of a sugar solution. If excessive bacteria ferment these sugars, the gases are absorbed into the bloodstream and exhaled, indicating SIBO.
- Jejunal Aspirate Culture:
- This invasive test involves taking a sample from the small intestine (via endoscopy) to directly measure bacterial concentration. Although considered the gold standard for diagnosis, it is rarely used due to its invasive nature.
Challenges in Diagnosing SIBO
- Overlap with Other Conditions: Symptoms of SIBO often overlap with Irritable Bowel Syndrome (IBS), Crohn’s disease, and lactose intolerance, making it difficult to differentiate between them based on symptoms alone.
- Breath Test Limitations: Breath tests are not always 100% accurate. False positives and false negatives can occur, leading to misdiagnosis or delays in treatment.
V. Treatment Strategies
1. Antibiotic Therapy
The cornerstone of treating SIBO is antibiotic therapy, aimed at reducing bacterial overgrowth. Some common antibiotics include:
- Rifaximin: A broad-spectrum, non-absorbable antibiotic that works in the gut to reduce bacterial overgrowth, particularly effective for hydrogen-producing bacteria.
- Neomycin: Often used in combination with rifaximin to target methane-producing bacteria.
However, antibiotic resistance and recurrence are common challenges. Many individuals experience a relapse of symptoms after the antibiotics are stopped.
2. Dietary Management
Diet plays a crucial role in managing SIBO. A diet aimed at reducing bacterial fermentation and supporting gut health can be very effective.
- Low FODMAP Diet: A diet low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) helps reduce the food sources available for the overgrown bacteria.
- Specific Carbohydrate Diet (SCD): This eliminates complex carbohydrates that bacteria thrive on, thus reducing symptoms.
- Gluten-Free Diet: For individuals with underlying celiac disease, a gluten-free diet is essential to prevent exacerbation of SIBO.
3. Alternative Treatments
- Probiotics: The role of probiotics in treating SIBO is controversial. While some evidence suggests that probiotics can help balance the gut microbiome, in some cases, they may exacerbate symptoms.
- Herbal Therapy: Herbal remedies like oregano oil, garlic, and berberine have shown antimicrobial properties and are sometimes used as alternatives to antibiotics for treating SIBO.
VI. Living with SIBO
1. Daily Management
Managing SIBO requires a combination of medication, diet, and lifestyle changes. These may include:
- Tailored Diets: Following a diet plan that reduces bacterial fermentation and supports gut health.
- Regular Follow-up: Ongoing medical support to adjust treatments as needed, especially if symptoms reoccur.
2. Long-Term Outlook
If untreated, SIBO can lead to severe complications such as malnutrition, vitamin deficiencies, and damage to the small intestine. However, with proper treatment and dietary modifications, many people can manage the symptoms and prevent long-term health issues.
VII. Future Directions
1. Research Trends
Ongoing research is exploring the connection between SIBO and other conditions like irritable bowel syndrome (IBS) and fibromyalgia. Studies on the gut microbiome’s role in SIBO are particularly promising and may lead to more targeted treatments in the future.
2. The Role of Technology
New technologies, such as next-generation sequencing for microbiome analysis, are helping researchers better understand the bacterial composition in the gut. This could lead to more personalized treatment plans for SIBO in the near future.
SIBO is a complex and often challenging condition to diagnose and treat, but with a proper understanding of its causes, symptoms, and treatment options, individuals can manage their symptoms effectively. Continued research into the gut microbiome and advancements in diagnostic technologies are essential for improving outcomes and making treatment more effective. By raising awareness and providing better educational resources, we can support those affected by SIBO and improve their quality of life.
How to Manage SIBO: A Comprehensive Guide for Patients

Small Intestinal Bacterial Overgrowth (SIBO) is a condition where excess bacteria grow in the small intestine, disrupting digestion and nutrient absorption. Managing SIBO requires a combination of recognizing its symptoms, treating it through dietary changes and medical interventions, and supporting digestive health in the long term. This guide aims to help patients understand the steps to manage SIBO and work with healthcare providers to achieve the best outcomes.
1. How to Recognize Symptoms of SIBO
Recognizing the symptoms of SIBO is the first step in managing the condition effectively. The most common symptoms include:
- Bloating and Abdominal Distension: One of the hallmark symptoms of SIBO is a feeling of fullness or bloating in the abdomen, often after eating.
- Abdominal Pain or Discomfort: Many individuals with SIBO experience cramping, sharp pain, or general discomfort, especially after meals.
- Diarrhea or Constipation: The bacterial overgrowth can disrupt normal gut motility, leading to either diarrhea or constipation, or a combination of both.
- Excessive Gas and Flatulence: As bacteria ferment undigested food in the small intestine, they produce gas, leading to increased burping and flatulence.
- Malabsorption and Nutritional Deficiencies: SIBO can interfere with the body’s ability to absorb essential nutrients, leading to symptoms like fatigue, weight loss, and deficiencies in vitamins such as B12 and fat-soluble vitamins (A, D, E, K).
- Fatigue and Brain Fog: Chronic malabsorption and the systemic effects of bacterial overgrowth can lead to fatigue, difficulty concentrating, and a feeling of mental fog.
- Heartburn or Acid Reflux: In some cases, the bacterial imbalance can trigger acid reflux, causing a burning sensation in the chest.
If you experience any combination of these symptoms, it’s important to seek medical advice for a proper diagnosis.
2. How to Treat SIBO: Dietary and Medical Approaches
SIBO is typically managed through a combination of dietary interventions and medical treatments. Both approaches aim to reduce bacterial overgrowth, support digestive health, and alleviate symptoms.
Dietary Approaches:
- Low FODMAP Diet:
- The low-FODMAP diet is one of the most effective dietary approaches for managing SIBO. FODMAPs are a group of carbohydrates that are poorly absorbed in the small intestine, and they can ferment in the gut, feeding the overgrown bacteria. By eliminating or reducing foods high in FODMAPs, such as certain fruits, dairy, and grains, patients can reduce fermentation and symptom severity.
- Specific Carbohydrate Diet (SCD):
- The SCD eliminates complex carbohydrates and sugars that feed harmful bacteria. It focuses on easily digestible carbohydrates, fruits, vegetables, and proteins. Many individuals with SIBO find relief from symptoms with this diet as it eliminates foods that may contribute to bacterial growth.
- Gluten-Free Diet:
- For individuals with celiac disease or gluten sensitivity, eliminating gluten is essential. Gluten can exacerbate gut inflammation and worsen SIBO symptoms.
- Probiotic and Prebiotic Management:
- The role of probiotics in treating SIBO is debated. In some cases, certain strains of probiotics may help balance the gut microbiota, while in others, they may worsen symptoms by promoting further bacterial growth. It is essential to discuss with your doctor whether probiotics are appropriate for your condition.
- Prebiotics—foods that feed healthy gut bacteria—should be introduced cautiously, as they can sometimes exacerbate symptoms in SIBO patients.
Medical Approaches:
- Antibiotic Therapy:
- Antibiotics are often prescribed to reduce the number of bacteria in the small intestine. Commonly used antibiotics for SIBO include:
- Rifaximin (commonly used for hydrogen-dominant SIBO)
- Neomycin (for methane-dominant SIBO)
- Metronidazole (in some cases)
- Antibiotics are typically effective in reducing symptoms, but SIBO often recurs once the medication is stopped, requiring ongoing management.
- Antibiotics are often prescribed to reduce the number of bacteria in the small intestine. Commonly used antibiotics for SIBO include:
- Herbal Antibiotics:
- Some patients prefer herbal antibiotics such as oregano oil, garlic extract, or berberine. These can have antimicrobial effects, but they should be used under the supervision of a healthcare provider to avoid overuse and resistance.
- Prokinetics:
- If motility issues contribute to the development of SIBO, prokinetic agents like low-dose erythromycin or prucalopride may be prescribed. These help improve gut motility, preventing the stasis that allows bacterial overgrowth.
- Nutrient Supplementation:
- If SIBO has led to malabsorption, your doctor may recommend nutrient supplementation (e.g., vitamin B12, iron, and fat-soluble vitamins) to address deficiencies and support overall health.
3. How to Support Digestive Health with SIBO
While antibiotics and diet changes are key to treating SIBO, there are several additional strategies you can adopt to support your digestive health:
- Hydration: Drink plenty of fluids, particularly water and electrolyte solutions, to help replenish fluids lost through diarrhea and vomiting. Proper hydration is essential for overall gut health and helps flush out toxins.
- Digestive Enzymes: Digestive enzymes may help improve nutrient absorption, particularly in cases of malabsorption, by supporting the breakdown of food in the small intestine.
- Stress Management: Chronic stress can impact gut health and exacerbate SIBO symptoms. Engaging in stress-reduction practices such as mindfulness, meditation, or yoga can help support your digestive health.
- Rest and Recovery: Your body needs time to heal from the strain SIBO places on your digestive system. Adequate sleep and rest are essential for the body to recover and support gut health.
4. How to Work with Your Doctor on SIBO Treatment
Successfully managing SIBO involves an ongoing partnership between you and your healthcare provider. Here’s how you can work together:
1. Proper diagnosis:
- If you suspect you have SIBO, it’s important to get a formal diagnosis. Your doctor may recommend breath tests or jejunal aspirate cultures to confirm the presence of bacterial overgrowth.
2. Tailored Treatment Plan:
- Work with your doctor to create a personalized treatment plan that addresses your unique symptoms and underlying conditions. This may involve choosing the right combination of antibiotics, dietary changes, and supplements.
3. Regular Follow-ups:
- SIBO often recurs, so regular follow-ups with your doctor are essential to monitor your progress. Follow-up visits allow your doctor to adjust your treatment plan and address any side effects or complications.
4. Managing Relapses:
- SIBO tends to relapse, so your doctor will guide you on how to manage recurring episodes. This may involve repeat antibiotic courses, further dietary modifications, and lifestyle adjustments.
5. Long-Term Maintenance:
- Once SIBO symptoms are under control, your doctor may help you develop a maintenance plan that includes a balanced diet, probiotics (if appropriate), and prokinetic therapy to prevent recurrence.
What is SIBO and How Does It Affect Health?
Small Intestinal Bacterial Overgrowth (SIBO) is a condition in which excessive bacteria grow in the small intestine, where the bacterial population is usually much lower compared to the colon. These bacteria, typically residing in the large intestine, can disrupt normal digestion and nutrient absorption when they overgrow in the small intestine. The excess bacteria ferment undigested food, producing gas, toxins, and other byproducts that can damage the lining of the small intestine, leading to malabsorption of nutrients and digestive discomfort.
SIBO can have a significant impact on health in various ways:
- Malabsorption of Nutrients: Overgrowth of bacteria interferes with the small intestine’s ability to absorb nutrients like vitamins (B12, A, D, and K), minerals (iron, calcium), and fatty acids, leading to deficiencies.
- Digestive disturbances: gas production from bacterial fermentation causes bloating, pain, and discomfort.
- Systemic Effects: Long-term SIBO can contribute to fatigue, joint pain, mental fog, and inflammation throughout the body due to nutritional deficiencies and the inflammatory response.
- Increased Risk of Other Health Issues: SIBO can exacerbate or be linked to other gastrointestinal conditions, such as Irritable Bowel Syndrome (IBS), Celiac Disease, or Crohn’s Disease.
What Are the Common Symptoms of SIBO?
SIBO manifests through a variety of symptoms, some of which overlap with other gastrointestinal issues like IBS or food sensitivities. Common symptoms include:
- Bloating and Abdominal Distension: A feeling of fullness or swelling in the abdomen, often worse after meals.
- Abdominal Pain and Cramping: Pain or discomfort in the stomach area, frequently triggered by eating.
- Excessive Gas and Flatulence: This results from the fermentation of food by the excess bacteria, leading to increased production of gas.
- Diarrhea and Constipation: SIBO can cause changes in bowel movements, either diarrhea (often after eating) or constipation, or a mixture of both.
- Malabsorption and Weight Loss: Difficulty absorbing nutrients from food leads to deficiencies in vitamins and minerals, which can result in weight loss, fatigue, and nutrient deficiencies.
- Fatigue and Brain Fog: Chronic fatigue, mental fog, and a lack of energy due to nutrient deficiencies and inflammation.
- Heartburn and acid reflux: In some cases, the overgrowth of bacteria can contribute to reflux and a burning sensation in the chest.
- Nutritional Deficiencies: Deficiencies in vitamin B12, iron, and fat-soluble vitamins (A, D, E, K) may occur due to bacterial interference with nutrient absorption.
How is SIBO diagnosed by healthcare professionals?
Diagnosing SIBO involves a combination of symptom evaluation, patient history, and diagnostic testing. While there is no single definitive test, healthcare professionals use several methods to confirm SIBO:
- Breath Tests:
- The lactulose breath test and glucose breath test are the most commonly used tests to diagnose SIBO. These tests measure the levels of hydrogen and methane gases in the breath after the patient consumes a sugar solution (lactulose or glucose). Elevated levels of these gases indicate bacterial overgrowth since bacteria ferment these sugars, releasing gas that is absorbed into the bloodstream and exhaled through the lungs.
- Hydrogen Breath Test: Measures hydrogen production, typically associated with hydrogen-dominant SIBO.
- Methane Breath Test: Measures methane production, which is often linked to methane-dominant SIBO.
- Jejunal Aspirate Culture:
- This is a more invasive test that involves collecting a sample of fluid from the small intestine using an endoscope. The fluid is cultured to directly count the number of bacteria. Although accurate, this method is less commonly used due to its invasive nature and the need for specialized equipment.
- Symptom Assessment:
- Healthcare providers will often assess symptoms like bloating, diarrhea, and pain to determine the likelihood of SIBO. Since symptoms overlap with other gastrointestinal disorders, further testing is usually needed to confirm the diagnosis.
What Lifestyle Changes Can Help Manage SIBO?
Managing SIBO requires a comprehensive approach that combines medical treatment, dietary modifications, and lifestyle changes. Here are some key lifestyle changes that can help manage SIBO:
- Stress Management:
- Chronic stress can disrupt gut motility and exacerbate SIBO symptoms. Incorporating stress reduction techniques, such as mindfulness, yoga, meditation, and regular physical activity, can help improve gut function and reduce symptoms.
- Regular Exercise:
- Moderate physical activity can help stimulate gut motility, reduce bloating, and promote overall digestive health. Aim for regular exercise like walking, swimming, or light strength training.
- Hydration:
- Staying hydrated is essential, especially for those experiencing diarrhea or vomiting. Drinking plenty of water and electrolyte drinks helps maintain fluid balance and supports digestive function.
- Avoid smoking and excessive alcohol.
- Smoking and excessive alcohol intake can exacerbate gut health issues and affect digestion. Quitting smoking and reducing alcohol consumption can contribute to improved digestive health and better management of SIBO.
- Sleep Hygiene:
- Getting adequate and restful sleep is vital for overall health, including gut health. Aim for 7–9 hours of sleep per night to allow the body to repair and support the immune system.
What Role Does Diet Play in Treating SIBO?
Diet plays a crucial role in managing SIBO by controlling bacterial growth, reducing symptoms, and promoting gut health. The following dietary strategies are commonly used to treat SIBO:
- Low FODMAP Diet:
- The Low FODMAP diet is one of the most well-known and widely recommended diets for SIBO. FODMAPs are a group of short-chain carbohydrates that are poorly absorbed in the small intestine and can ferment, feeding bacteria. Reducing the intake of high-FODMAP foods (such as certain fruits, vegetables, dairy, and grains) helps minimize bacterial fermentation and reduce symptoms like bloating and gas.
- Specific Carbohydrate Diet (SCD):
- The Specific Carbohydrate Diet eliminates complex carbohydrates, processed foods, and sugars that feed harmful bacteria. It emphasizes easily digestible whole foods such as lean proteins, fruits, and vegetables and can be an effective way to reduce bacterial overgrowth.
- Gluten-Free Diet:
- For individuals with celiac disease or gluten sensitivity, a gluten-free diet is essential. Even for those without celiac disease, reducing gluten may help decrease inflammation in the gut and support healing.
- Fermented Foods:
- While fermented foods (e.g., sauerkraut, kimchi, kefir) are generally beneficial for gut health, they may not be suitable for individuals with SIBO. These foods contain high levels of bacteria and may aggravate symptoms by increasing the bacterial load in the gut.
- Intermittent Fasting:
- Some people with SIBO find relief by practicing intermittent fasting, which gives the digestive system time to rest between meals. This may help reduce bacterial fermentation and improve digestion.
- Supplementation:
- Certain nutritional supplements, such as digestive enzymes or probiotics (in some cases), may help improve digestion and balance gut bacteria. However, probiotics should be used cautiously, as they can sometimes exacerbate symptoms in individuals with SIBO.
- Avoiding excessive sugar:
- A diet high in sugar can feed bacteria in the small intestine, exacerbating SIBO symptoms. Reducing sugar and refined carbohydrates can help starve off the overgrown bacteria.
SIBO is a complex condition that requires a multi-faceted approach for management. Recognizing the symptoms, getting a proper diagnosis, and making necessary lifestyle and dietary changes can significantly improve the quality of life for individuals with SIBO. With the right combination of medical treatment, diet, and lifestyle modifications, it is possible to manage SIBO effectively and minimize its impact on health. Always consult a healthcare provider before making any significant changes to diet or treatment.
Conclusion
Managing SIBO requires a multi-faceted approach involving both medical treatment and lifestyle adjustments. By recognizing symptoms early, working closely with your healthcare provider to develop a personalized treatment plan, and supporting your digestive health with dietary changes, supplements, and stress management, you can significantly improve your quality of life. Keep in mind that SIBO may require ongoing management, and staying informed about your condition will help you work effectively with your healthcare provider to maintain optimal digestive health.