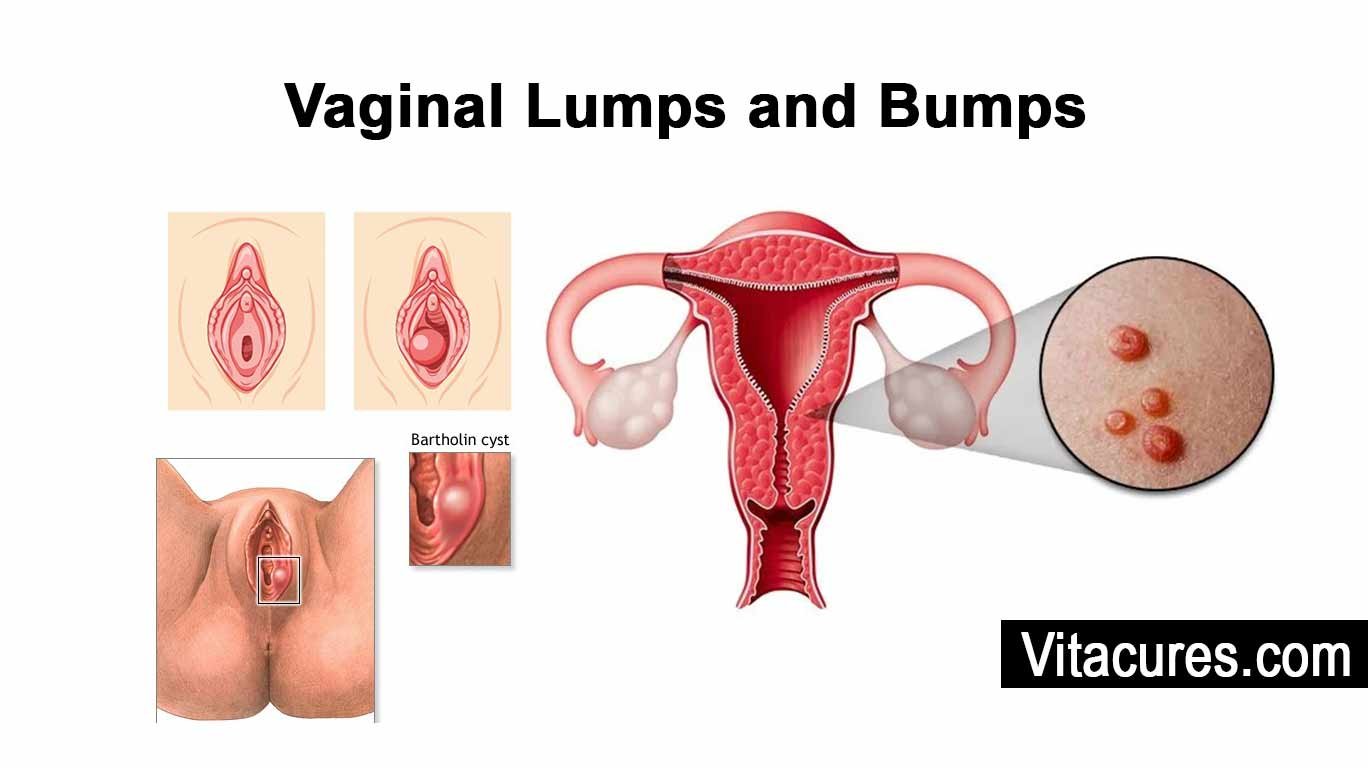
Vaginal lumps and bumps are growths or swellings that appear on or inside the vaginal area. These can vary widely in size, color, and texture, and might be a single bump or several grouped together. They can be a normal part of the body or a sign of a medical condition that needs attention. Understanding what these lumps and bumps are, why they occur, and when to seek medical advice is crucial for maintaining vaginal health.
What are Vaginal Lumps and Bumps?
Vaginal lumps and bumps are little growths that can pop up on or inside the vaginal area. They can look and feel different from each other—some are soft, some are hard, and they can be alone or in groups. It’s really important to know about these because while many are nothing to worry about, some need a doctor’s attention.
These bumps can happen for a bunch of reasons. You might get them from an infection like HPV, which causes genital warts, or from something simpler like an ingrown hair from shaving. Hormone changes from your period, pregnancy, or menopause can also cause them. Usually, they’re no big deal, but it’s good to keep an eye on them just in case.
If you spot a bump, keep track of it, especially if it doesn’t go away, starts to hurt, itch, bleed, or gives off a weird discharge. If you see these signs, it’s a good idea to check in with your doctor. They’ll take a look, ask some questions, and might run some tests to figure out what’s up. This way, you’ll know exactly what you’re dealing with.
How to treat these bumps depends on what’s causing them. Sometimes, just keeping the area clean and using a warm compress is enough. If it’s an infection, you might need medicine. And if the bump is big and bothersome, you might need a small procedure to take it out. Regular visits to your gynecologist and good hygiene can help prevent these bumps, or at least catch them early when they’re easier to treat.
Vaginal Bumps and Their Causes
- Vaginal lumps and bumps are small growths that can appear on or inside the vaginal area.
- They can be soft, hard, and can be alone or in groups.
- Causes include infections like HPV, ingrown hair from shaving, hormonal changes from period, pregnancy, or menopause.
- Observing these bumps is crucial, especially if they persist, hurt, itch, bleed, or discharge unusual discharges.
- Treatment depends on the cause, including cleaning and warm compressing, medication, or a small procedure.
- Regular gynecologist visits and good hygiene can help prevent or catch these bumps early.
Read More: vaginal depth / Vaginal Pump / Vaginal Cuff / Vaginal Dryness / Tighten Your Vagina / Sore Penis After Sex / Nicotine and Your Sex Drive / Why am I so horny? / Sexual Battery
Vagina vs. vulva
The terms “vagina” and “vulva” are often used interchangeably, but they refer to different parts of the female anatomy.
Vagina
The vagina is an internal organ that is part of the female reproductive system. It’s a muscular canal that runs from the cervix, the lower part of the uterus, to the outside of the body. The primary functions of the vagina include facilitating menstrual flow, sexual intercourse, and childbirth. It’s also involved in the natural self-cleaning process, maintaining a balance of healthy bacteria and pH levels to prevent infections.
Vulva
The vulva refers to the external part of the female genitalia. It includes several structures:
- Labia Majora: The outer lips of the vulva, which are usually covered with pubic hair.
- Labia Minora: The inner lips, which can vary greatly in size and color from one woman to another.
- Clitoris: A small, sensitive protrusion located at the top of the vulva, known for its role in female sexual pleasure.
- Urethral Opening: Located just above the vaginal opening, through which urine exits the body.
- Vaginal Opening: Also known as the introitus, this is the entrance to the vagina.
- Bartholin’s Glands: Located on either side of the vaginal opening, these glands produce fluid that lubricates the vulva.
Importance of Understanding the Difference
Knowing the difference between the vagina and vulva is important for health, medical, and educational purposes. It helps in understanding female anatomy accurately, discussing health issues precisely, and ensuring proper healthcare and hygiene. Misunderstandings can lead to confusion in medical contexts and may impact the effectiveness of communication about health issues, treatments, and hygiene practices.
Causes of Vaginal Lumps and Bumps
Vaginal lumps and bumps can appear for various reasons, and infections are one of the most common causes. Understanding the different types of infections can help you identify potential issues early and seek appropriate treatment. Here’s a look at some of the infections that might lead to the development of vaginal lumps and bumps:
Fungal Infections
One common type of infection that can cause vaginal bumps is a fungal infection, such as a yeast infection. These infections are caused by an overgrowth of yeast, a type of fungus, which can lead to irritation, swelling, and sometimes lumps in the vaginal area. Symptoms typically include itching, redness, and a thick, white discharge that resembles cottage cheese. Yeast infections can cause discomfort and an increase in the size of the labia, which might feel like bumps.
Bacterial Infections
Bacterial infections can also lead to vaginal lumps and bumps. One common bacterial condition is bacterial vaginosis (BV), which occurs when there is an imbalance of the natural bacteria in the vagina. Although BV itself doesn’t usually cause lumps, it can lead to inflammation and changes in the vaginal area that might feel like bumps. Another bacterial infection, such as a Staphylococcus or Streptococcus infection, might cause boils or abscesses in the vaginal area, which are painful, pus-filled lumps.
Sexually Transmitted Infections (STIs)
STIs are a significant cause of vaginal lumps and bumps. For example:
- Genital Herpes: This STI causes painful sores that might start as small red bumps before turning into blisters and then scabbing over.
- Genital Warts: Caused by the human papillomavirus (HPV), genital warts can appear as small, flesh-colored bumps or groups of bumps in the genital area. They can be small or large, raised or flat, or shaped like a cauliflower.
- Syphilis: The initial sign of syphilis is typically a small, painless sore called a chancre. While it can appear anywhere on the body that has been exposed to the bacterium, on the genitals, it might be mistaken for a bump or lump.
Vaginal Bumps and Infections Overview
- Fungal Infections: Common cause of vaginal bumps due to yeast overgrowth, causing irritation, swelling, and lumps. Symptoms include itching, redness, and thick white discharge.
- Bacterial Infections: Cause inflammation and changes in the vaginal area. Staphylococcus or Streptococcus infections can cause painful, pus-filled lumps.
- Sexually Transmitted Infections (STIs): Significant causes of vaginal lumps and bumps.
- Early recognition and proper treatment are crucial for effective management and prevention of complications.
Each of these infections has its specific symptoms and treatments, so it’s important to consult a healthcare provider if you suspect you have an STI or any infection causing bumps or lumps in the vaginal area. Recognizing these symptoms early and getting proper treatment can help manage the conditions effectively and prevent complications.
Cysts
Cysts are another common cause of vaginal lumps and bumps, arising from fluid, air, or other substances building up inside a pocket in the skin or underlying tissues. In the vaginal area, cysts can develop in several ways and can vary greatly in terms of size and severity.
Bartholin Cysts
One of the most well-known types of cysts in the vaginal area is the Bartholin cyst, which forms when the ducts of the Bartholin glands become blocked. These glands are located on each side of the vaginal opening and produce fluid that helps lubricate the vagina. When the ducts are blocked, fluid backs up into the gland, leading to the formation of a cyst. A Bartholin cyst can be painless and small, but if infected, it can turn into an abscess, which is usually painful and large. If a Bartholin cyst becomes too large or causes significant discomfort, treatment might involve a minor procedure to drain the cyst or surgery to remove it entirely.
Other Types of Cysts
In addition to Bartholin cysts, several other types of cysts can occur in the vaginal area:
- Epidermoid Cysts: These are relatively common and arise from the skin cells on or under the skin. Unlike Bartholin cysts, epidermoid cysts are not related to glands but rather develop when the skin turns inward, trapping skin cells. These cysts can appear anywhere on the skin, including the genital area, and are typically benign.
- Skene’s Duct Cysts: These cysts develop near the entrance of the vagina, closer to the urethra, where the Skene’s glands are located. These glands are involved in lubricating the urethra and can become blocked, leading to cyst formation.
- Inclusion Cysts: Often resulting from an injury to the vaginal walls, such as those that can occur during childbirth or surgery, inclusion cysts are formed when the skin cells are trapped beneath the surface of the vaginal lining.
- Gartner’s Duct Cysts: These are vaginal cysts that can form from remnants of the ducts from the developmental stage. They are generally located along the side walls of the vagina and are usually harmless unless they grow large enough to cause discomfort.
Most cysts are benign and may not require treatment unless they cause discomfort, become infected, or grow unusually large. Treatment options include surgical removal, draining, and, in some cases, simply monitoring the cyst over time. It’s important to consult with a healthcare provider for a proper diagnosis and appropriate management of any cysts in the vaginal area.
Vaginal Cysts Overview
- Common cause of vaginal lumps and bumps.
- Types vary in size and severity.
- Bartholin Cysts: Form when ducts of Bartholin glands become blocked.
- Treatment may involve minor procedure or surgery.
- Other types include Epidermoid Cysts, Skene’s Duct Cysts, Inclusion Cysts, and Gardner’s Duct Cysts.
- Most cysts are benign and may not require treatment unless they cause discomfort, become infected, or grow large.
- Treatment options include surgical removal, draining, and monitoring.
Skin Conditions
Various skin conditions can lead to the development of vaginal lumps and bumps, affecting the appearance and health of the skin in the vaginal area. Here’s an overview of some common skin conditions that might manifest as lumps or bumps in the genital region:
Dermatitis
Dermatitis is an inflammation of the skin that can cause itching, redness, and irritation. In the vaginal area, this can occur due to several factors:
- Contact Dermatitis: This form arises from an allergic reaction or irritation caused by direct contact with allergens or irritants such as scented soaps, detergents, or fabric softeners used on underwear. Symptoms include redness, itching, and sometimes the formation of small bumps or blisters.
- Seborrheic Dermatitis: This type usually affects areas of the skin where oil glands are prominent, such as the scalp and face, but can also appear in the genital area, causing red, scaly patches.
Psoriasis
Psoriasis is a chronic autoimmune condition characterized by the rapid buildup of skin cells that leads to scaling on the skin’s surface. These scales are typically white-silver and develop in thick, red patches. Occasionally, they can crack and bleed. In the genital area, psoriasis can be particularly uncomfortable and may appear as red, non-scaly patches. This area often responds well to treatments, but due to the sensitive nature of the skin, treatment options may differ from those used on other body parts.
Lichen Sclerosus
Lichen sclerosis is a rare, chronic skin condition that creates thin, white, crinkly patches on the skin, which can become sore or itchy. It’s most commonly seen on the genital and anal regions and can affect women of any age. If untreated, lichen sclerosis may lead to scarring, which can cause pain, changes in the shape of the genital area, and difficulties with sexual intercourse or urination. Early diagnosis and treatment are important to manage symptoms and prevent complications.
Each of these conditions requires different management strategies, which might include:
- Topical Treatments: Creams and ointments, including corticosteroids or newer non-steroidal topical treatments, are often used to reduce inflammation and treat symptoms.
- Systemic Medications: For severe cases, especially with psoriasis or lichen sclerosus, systemic medications that affect the whole body may be necessary.
- Lifestyle Adjustments: Avoiding known irritants, using gentle hygiene products, and wearing loose, breathable clothing can help manage symptoms.
It’s crucial for individuals experiencing symptoms of these skin conditions to consult with a healthcare provider who can provide a proper diagnosis and appropriate treatment plan. Timely and effective treatment can help manage the symptoms, improve skin health, and enhance the quality of life.
Vaginal Skin Conditions and Impact
- Dermatitis: Inflammation causing itching, redness, and irritation.
- Seborrheic Dermatitis: Usually affects areas with prominent oil glands and can also appear in the genital area.
- Psoriasis: Chronic autoimmune condition causing rapid skin cell buildup leading to scaling.
- Lichen Sclerosus: Rare, chronic skin condition causing thin, white, crinkly patches.
- Management Strategies: Topical treatments, systemic medications, lifestyle adjustments.
- Consultation with a healthcare provider is crucial for proper diagnosis and treatment.
Benign Growths
Benign growths in the vaginal area can take several forms, including fibromas and polyps. These types of growths are non-cancerous but can cause discomfort or concern due to their presence. Understanding what they are and how they can affect your health is important for managing them appropriately.
Fibromas
Fibromas, also known as fibroid tumors or leiomyomas when they occur in the uterus, are benign tumors made up of fibrous or connective tissue. In the vaginal area, fibromas can appear as firm, rubbery lumps that are usually painless. They can vary in size from very small to quite large. Fibromas are typically slow-growing and often remain stable without causing any symptoms or health issues. However, if a fibroma becomes large or located in a spot that causes irritation or discomfort, medical treatment might be necessary. Treatment options can include surgical removal if the fibroma causes significant discomfort or disrupts normal function.
Polyps
Polyps are another type of benign growth that can appear in the vaginal area, commonly arising from the lining of the vagina or cervix. Vaginal and cervical polyps are soft, usually painless, and often appear on a stalk. They can be red, pink, or gray in color and vary in size. Polyps are generally asymptomatic but can sometimes cause symptoms such as irregular bleeding, especially after intercourse, or an unusual discharge if they become irritated.
The exact cause of polyps is not well understood, but they are associated with increased levels of estrogen, inflammation, or clogged blood vessels in the cervix or vaginal wall. Polyps are usually discovered during routine pelvic examinations or evaluations for symptoms such as abnormal bleeding.
Treatment and Management
The treatment for benign growths like fibromas and polyps often depends on their size, location, and the symptoms they cause:
- Observation: Small growths that cause no symptoms might not require immediate treatment and can be monitored over time.
- Surgical Removal: For polyps, removal is typically a simple procedure that can be done in a doctor’s office under local anesthesia. This is often recommended if there’s concern about the nature of the growth or if it causes symptoms.
- Medication: In some cases, particularly with fibromas, medications that regulate hormone levels can help reduce symptoms or slow the growth’s progression.
If you suspect you have a benign growth like a fibroma or polyp, it’s important to see a healthcare provider for a diagnosis. They can assess the growth and determine the best course of action based on your individual health needs. Most benign growths are easily manageable with medical guidance, ensuring they don’t impact your overall health and quality of life.
Malignant conditions of the vaginal area, including various types of cancers, are serious health concerns that require immediate medical attention. Early detection and treatment are crucial for the best outcomes. Below, we discuss some of these conditions, focusing primarily on vaginal cancer and other related cancers that can affect the vaginal area.
Malignant Conditions
Vaginal Cancer
Vaginal cancer is relatively rare and occurs when malignant (cancerous) cells form in the tissues of the vagina, the muscular tube connecting the cervix and the vulva. It’s more commonly found in women over the age of 60, but it can occur at any age.
Types of Vaginal Cancer
- Squamous Cell Carcinoma: This is the most common type of vaginal cancer, originating in the squamous cells that line the vagina. It typically develops slowly and is often found in women who have a history of cervical cancer or precancerous cervical lesions.
- Adenocarcinoma: This type begins in the glandular cells of the vagina that produce fluids. Adenocarcinoma is more likely to spread to the lungs and lymph nodes than squamous cell carcinoma.
- Melanoma: A less common type that starts in the pigment-producing cells of the skin or the mucosal surfaces lining the vagina.
- Sarcoma: Rare in adults, these grow in the connective tissue or muscle layers of the walls of the vagina, usually affecting younger women or children.
Symptoms
Symptoms of vaginal cancer might include abnormal vaginal bleeding (especially after intercourse), watery vaginal discharge, a lump or mass in the vagina that can be felt, pain during intercourse, or frequent urination.
Treatment
Treatment options depend on the type, size, and stage of the cancer and may include surgery, radiation therapy, and chemotherapy.
Other Cancers Affecting the Vaginal Area
Other cancers can also affect the vaginal area, either by originating in nearby structures or by metastasizing (spreading) from other parts of the body:
- Cervical Cancer: Often associated with the human papillomavirus (HPV), cervical cancer can cause lesions on the cervix that, if untreated, may spread to the vagina.
- Vulvar Cancer: This starts in the vulva, the outer part of the female genital organs. It can cause symptoms like itching, burning, or bleeding, and lesions or lumps on the vulva.
- Endometrial (Uterine) Cancer: Cancer that starts in the lining of the uterus can spread to the vagina. Symptoms might include abnormal vaginal bleeding, pelvic pain, and a mass in the pelvic area.
- Ovarian Cancer: While ovarian cancer primarily affects the ovaries, it can metastasize to other parts of the pelvic region, including the vagina.
Importance of Screening and Early Detection
Regular pelvic exams and Pap tests are crucial for detecting precancerous conditions and cancers in their early stages, especially cervical cancer, which can lead to vaginal cancer. Women should discuss their risk factors with a healthcare provider, who may suggest additional tests or preventive measures like the HPV vaccine.
If any unusual symptoms occur, such as unexpected vaginal bleeding, discharge, or pain, it’s important to consult a healthcare provider promptly. Early diagnosis and treatment can significantly improve the prognosis of malignant conditions in the vaginal area.
Physical Symptoms of Vaginal Lumps and Bumps
Vaginal lumps and bumps can manifest a range of physical symptoms depending on their underlying cause. Commonly, you might notice a noticeable lump or swelling in the vaginal area, which could be singular or multiple. These can vary greatly in terms of size, texture, and tenderness. Some lumps might be soft and painless, while others can be hard and cause discomfort or pain, especially when touched or during activities like walking, sitting, or during sexual intercourse.
Other physical symptoms can include itching or irritation around the affected area. In cases of infections like genital herpes or HPV, these bumps might be accompanied by other symptoms such as redness, a burning sensation, or unusual discharge. Some bumps, particularly those that become infected, might also produce pus or bleed.
Emotional Impact
The presence of vaginal lumps and bumps can also have a significant emotional or psychological impact. Discovering any unexpected change in your body can be distressing. Many women feel anxiety or fear about the appearance and potential health implications of these bumps. Concerns about sexual health and the reaction of a sexual partner can also lead to feelings of embarrassment or a decreased desire for intimacy, potentially impacting personal relationships.
It’s not uncommon for these concerns to escalate into stress or anxiety, especially if the cause of the lump or bump is unknown or if one assumes the worst. Emotional support and clear communication with a healthcare provider can help alleviate these fears by providing reassurance and accurate information about the condition and its management.
When to Seek Medical Attention
It’s crucial to know when to seek medical attention for vaginal lumps and bumps. You should consult a healthcare provider if:
- The lump appears suddenly or changes quickly in size or shape.
- You experience persistent pain, itching, redness, or irritation that does not improve with basic home care.
- There are symptoms of infection, such as fever, pus, or an unusual discharge.
- The lump interferes with your daily activities, including sexual intercourse, walking, or using the bathroom.
- You notice bleeding not associated with your menstrual cycle.
Additionally, any persistent lump or bump that doesn’t resolve on its own within a few weeks should be evaluated by a professional. Early diagnosis and treatment can prevent potential complications and provide peace of mind. Remember, it’s always better to be safe and get any unexplained changes checked out, as early detection often leads to more effective treatment.
Diagnosis of Vaginal Lumps and Bumps
When it comes to diagnosing vaginal lumps and bumps, a comprehensive approach is typically taken, involving a physical examination, a review of medical history, and possibly diagnostic tests. Understanding each step can help you feel more prepared and informed about the process.
Physical Examination
The first step in diagnosing vaginal lumps and bumps is usually a thorough physical examination. Your healthcare provider will visually inspect the vaginal area for any noticeable lumps, bumps, discoloration, or other abnormalities. They might also feel the area to determine the texture, size, and location of any growths. This examination might extend to the pelvic area to check the internal reproductive organs and nearby tissues. This initial check helps to assess the general state of your vaginal health and identify any visible concerns.
Medical History
Taking a detailed medical history is another crucial step. Your healthcare provider will ask about your symptoms, any recent changes in your health, sexual history, and any past medical treatments. They’ll also inquire about any related symptoms, like pain, itching, or discharge, which could indicate an underlying condition. Your answers can provide clues about potential causes of the lumps or bumps, such as infections, hormonal changes, or other health issues.
Diagnostic Tests
Depending on the findings from the physical examination and medical history, specific diagnostic tests might be recommended:
- Ultrasound: This imaging test uses sound waves to create pictures of the inside of the body. It can be particularly useful if the lump is not easily accessible or visible. An ultrasound can help differentiate between different types of growths, such as cysts or solid tumors, and can also assess other pelvic organs.
- Biopsy: A biopsy involves taking a small sample of tissue from the lump, which is then examined under a microscope. This test is crucial for determining if a growth is benign or malignant and identifying the specific type of cells involved. A biopsy can provide definitive information, helping to guide treatment decisions.
Importance of Diagnosis
Accurate diagnosis of vaginal lumps and bumps is essential for effective treatment. It helps determine whether the condition is something benign that can be monitored or treated with simple interventions, or if it requires more aggressive treatment to manage a potentially serious condition. By combining a physical exam, medical history, and appropriate diagnostic tests, healthcare providers can develop a tailored approach to treat and manage any identified issues effectively.
If you notice any new or changing lumps in your vaginal area, it’s important to consult with a healthcare provider promptly to get a proper diagnosis and ensure your peace of mind.
Treatment Options for Vaginal Lumps and Bumps
Treating vaginal lumps and bumps effectively depends on accurately diagnosing their cause. Treatment can range from simple home remedies to more involved medical interventions, including medications, procedures, or surgery. Here’s an overview of the potential treatment options:
Home Remedies
For minor and non-serious bumps, such as those caused by irritation or mild infections, home remedies can be effective:
- Warm Compresses: Applying a warm, wet compress to the area can help reduce pain and swelling, especially for cysts like Bartholin’s cysts that are not infected.
- Sitz Baths: Soaking in a shallow bath that covers the pelvic area can help relieve symptoms and promote healing.
- Good Hygiene: Keeping the vaginal area clean and dry is crucial. Use mild, unscented soap and avoid irritating agents like scented wipes or douches.
- Loose Clothing: Wearing loose, breathable clothing can reduce irritation and allow the area to heal.
Medical Treatments
When home remedies are not enough, or when the cause of the lumps and bumps is more severe, medical treatments may be necessary:
- Medications:
- Antibiotics: If the lump is caused by a bacterial infection, antibiotics can clear the infection and reduce swelling.
- Antiviral Medication: For bumps caused by viral infections like genital herpes, antiviral medications can help manage outbreaks.
- Hormonal Treatments: In cases where hormonal imbalance is suspected, such as with certain types of cysts, hormonal medications may help regulate hormone levels and reduce symptoms.
- Procedures:
- Drainage: Some cysts, like Bartholin’s cysts, may require drainage if they are large, painful, or infected. This is a simple procedure that can be performed in a doctor’s office.
- Cryotherapy: Used primarily for genital warts, this procedure involves freezing the bumps to remove them.
- Laser Therapy: This can be used to remove or reduce the size of lumps and improve cosmetic appearance, particularly with persistent genital warts or other non-cancerous growths.
When Surgery is Necessary
Surgery may be required in certain situations, particularly when the growths are suspicious, potentially cancerous, or when they repeatedly cause symptoms despite other treatments:
- Excision: Removing the lump surgically is often a straightforward procedure that can be done under local anesthesia, particularly for benign growths like cysts or fibromas.
- Cancer Treatment: If a biopsy indicates cancerous growths, more extensive surgical interventions might be necessary, depending on the type and stage of the cancer. This might include removing part or all of the affected organs, followed by radiation or chemotherapy.
The right treatment for vaginal lumps and bumps varies greatly depending on the underlying cause. It’s important for individuals experiencing these symptoms to consult with healthcare professionals who can provide a diagnosis and recommend appropriate treatment options. Regular monitoring and follow-up care are crucial, especially if the condition persists or worsens, to ensure effective management and maintain overall health.
What is Molluscum Contagiosum?
Molluscum contagiosum is a common, contagious skin infection caused by the molluscum contagiosum virus, a type of poxvirus. It primarily affects children, but it can also occur in adults, particularly those with weakened immune systems or through sexual contact. The infection is characterized by the appearance of small, round, and painless bumps on the skin.
Symptoms of Molluscum Contagiosum
The primary symptom of molluscum contagiosum is the appearance of small, firm bumps on the skin. These bumps are usually:
- Small in size, typically between 2 to 5 millimeters in diameter.
- Pearly or flesh-colored, sometimes with a central dimple.
- Smooth and round in shape.
- Painless, but they can become itchy, red, or swollen if irritated or infected.
The bumps can appear anywhere on the body but are commonly found on the trunk, arms, legs, groin, and genital area in adults. In children, they tend to appear on the face, trunk, and limbs. The bumps may appear in clusters and can spread across different parts of the body through self-contamination from scratching or through direct contact with infected skin.
Treatment for Molluscum Contagiosum
Molluscum contagiosum typically resolves on its own without treatment within 6 to 12 months; however, new lesions may continue to appear as old ones fade. If the lesions are in sensitive areas, are causing discomfort, or if there is an underlying immune compromise, treatment might be necessary to speed up resolution and prevent further spread. Treatment options include:
- Physical Removal:
- Cryotherapy: Freezing the bumps with liquid nitrogen.
- Curettage: Scooping out the bumps with a small tool.
- Laser Therapy: Using a laser to destroy the bumps.
- Topical Treatments:
- Imiquimod Cream: An immune response modifier that stimulates the body’s immune system to fight off the virus.
- Podophyllotoxin Cream: A plant-based antiviral that helps to destroy the tissue of the bumps.
- Cantharidin: A chemical derived from the blister beetle, which is applied by a healthcare provider and causes the skin under the bump to blister and shed.
- Home Care:
- Avoiding scratching or picking at the bumps to prevent the spread of the virus to other parts of the body or to other people.
- Keeping the affected area clean and covered with clothing or a bandage to minimize the risk of transmission.
In cases where molluscum contagiosum is widespread or persistent, especially in immunocompromised individuals, consultation with a dermatologist or infectious disease specialist may be advisable for more aggressive treatment options.
Overall, while molluscum contagiosum is typically a minor infection, understanding its symptoms and treatment options can help manage the condition more effectively and prevent its spread to others.
Prevention Tips for Molluscum Contagiosum
Preventing molluscum contagiosum largely involves good hygiene practices, safe sexual behaviors, and regular health check-ups. Here are detailed strategies in each category:
Hygiene Practices
Good hygiene is critical in preventing the spread of molluscum contagiosum, especially among children, who are more likely to get the infection due to closer physical contact during play and less awareness about personal space.
- Personal Items: Avoid sharing towels, clothes, bed linens, or other personal items that may have come into contact with the bumps.
- Hand Washing: Frequent and thorough hand washing is crucial, especially after touching the affected areas of the skin.
- Covering the Bumps: Keep the bumps covered with clothing or waterproof bandages when in public settings or when there is a risk of skin-to-skin contact.
- Clean Environment: Regularly clean and disinfect surfaces that are frequently touched, such as toys, doorknobs, and bathroom fixtures, to reduce the risk of viral transmission.
Safe Sexual Practices
Since molluscum contagiosum can also be transmitted through sexual contact, practicing safe sex is an important preventive measure for sexually active adults.
- Barrier Protection: Use condoms and dental dams to reduce the risk of skin-to-skin contact with the bumps during sexual activity.
- Avoid Contact: Avoid sexual contact with anyone who has visible bumps or who has been diagnosed with molluscum contagiosum until they have been treated and the bumps have resolved.
- Communication: Maintain open communication with sexual partners about any current or past infections and encourage them to be honest about their own health status.
Regular Check-ups
Regular medical check-ups can help catch and address molluscum contagiosum early, especially in children or in individuals who have weakened immune systems.
- Routine Skin Exams: Include skin examinations as part of regular health check-ups, especially for children and individuals with eczema, who are more susceptible to infections like molluscum contagiosum.
- Prompt Treatment: If molluscum contagiosum is diagnosed, follow the treatment advice of healthcare providers promptly to minimize the risk of spreading the virus to others.
- Monitor for Complications: Regular check-ups can help ensure that any complications or secondary infections are treated promptly, reducing the risk of more serious health issues.
By adhering to these preventive tips, individuals can significantly reduce their risk of contracting or spreading molluscum contagiosum. Hygiene, safe sexual practices, and regular health check-ups are key components of preventing not only molluscum but also many other communicable diseases.
FAQs about Vaginal Lumps and Bumps
Vaginal lumps and bumps are a common concern for many women, leading to various questions and some misinformation. Here are answers to some frequently asked questions along with clarifications on common myths.
Common Questions and Answers
Q1: What are the most common causes of vaginal lumps and bumps?
A1: The most common causes include benign conditions such as cysts (like Bartholin’s or sebaceous cysts), infections (like genital warts or herpes), and other skin conditions (like ingrown hairs or dermatitis). Malignant causes are less common but include vaginal cancer.
Q2: Are vaginal lumps and bumps always a sign of an STD?
A2: No, not always. While sexually transmitted diseases (STDs) like genital warts and herpes can cause lumps and bumps, many other non-STD causes exist, such as cysts, blocked glands, or benign skin conditions.
Q3: Can vaginal lumps and bumps be prevented?
A3: While not all can be prevented, reducing the risk is possible through good hygiene, safe sexual practices, and regular medical check-ups. Avoiding shared personal items and keeping the genital area clean and dry can also help.
Q4: When should I see a doctor for vaginal lumps and bumps?
A4: You should see a doctor if the bumps are painful, multiply, or change in appearance, or if they are accompanied by other symptoms like bleeding, discharge, or itching. It’s also important to seek medical advice if the bumps do not go away on their own after a few weeks.
Misinformation and Myths
Myth 1: Vaginal lumps are always cancerous.
Fact: Most vaginal lumps are benign and not cancerous. Conditions like cysts and benign tumors are common, and even infectious causes are often treatable. However, any persistent lump should be evaluated by a healthcare provider.
Myth 2: You can treat vaginal lumps with over-the-counter creams.
Fact: While some minor issues like irritated skin might benefit from over-the-counter treatments, most causes of vaginal lumps require specific treatments that are not available OTC. It’s important to have a proper diagnosis before starting any treatment.
Myth 3: Vaginal lumps are a sign of poor hygiene.
Fact: Many causes of vaginal lumps, such as cysts or hormonal changes, are not related to hygiene. While maintaining good hygiene can help prevent infections, it does not guarantee that you will never develop lumps or bumps.
Myth 4: If you have vaginal lumps, you should stop having sex.
Fact: Not all vaginal lumps and bumps necessitate abstaining from sexual activity. However, if the lumps are due to an infectious cause like genital herpes or warts, it’s important to avoid sexual contact to prevent spreading the infection to partners. Always consult with a healthcare provider for advice tailored to your specific condition.
These FAQs and myth-busting facts can help clear up some of the common misunderstandings about vaginal lumps and bumps and encourage women to seek appropriate medical advice when needed.
Resources and Support for Dealing with Vaginal Lumps and Bumps
Navigating the concerns and treatment of vaginal lumps and bumps can be challenging, but there are many resources and support systems available. Here’s how you can find support, further your knowledge, and get professional help.
Support Groups
Joining a support group can be invaluable, providing emotional support and practical advice from others who have faced similar issues. Here are a few options:
- Online Forums: Websites like Women’s Health Forum or HealthBoards offer specific sections for discussions about gynecological issues, where you can share experiences and receive support from peers.
- Local Support Groups: Some hospitals or community centers host support groups for women dealing with various health issues, including reproductive health concerns. Ask your healthcare provider for recommendations.
- Social Media Groups: Platforms like Facebook and Reddit have communities or subreddits focused on women’s health where members discuss their experiences and support each other.
Recommended Reading
Educating yourself about vaginal health can help you make informed decisions. Some recommended books and websites include:
- “The V Book: A Doctor’s Guide to Complete Vulvovaginal Health” by Elizabeth G. Stewart: This book offers comprehensive information on a wide range of vaginal health issues, including lumps and bumps.
- Centers for Disease Control and Prevention (CDC) Website: The CDC provides resources and information on sexually transmitted infections, which can cause vaginal lumps.
- The American College of Obstetricians and Gynecologists (ACOG) Website: ACOG offers valuable patient education resources that can help you understand various conditions affecting vaginal health.
Professional Help
If you’re dealing with vaginal lumps and bumps, it’s crucial to seek professional medical advice. Here’s how to get help:
- Gynecologist: A gynecologist specializes in female reproductive health and is the best person to consult for any vaginal health issues. They can provide diagnoses, treatments, and referrals if necessary.
- Dermatologist: For skin-related issues like dermatitis or infectious bumps, visiting a dermatologist might be beneficial.
- Infectious Disease Specialist: If an infectious cause is suspected, such as an STI, consulting with an infectious disease specialist can provide targeted treatment.
If you’re unsure where to start, your primary care provider can guide you to the appropriate specialist based on your symptoms and concerns. Remember, professional healthcare providers are your best resource for accurate diagnosis and effective treatment. Engaging with a support network and educating yourself can also help you navigate the challenges of vaginal lumps and bumps more effectively.